Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Coumadin PT Ed 2013
Cargado por
api-241616443Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Coumadin PT Ed 2013
Cargado por
api-241616443Copyright:
Formatos disponibles
Anticoagulation Service Washington Health System Cardiovascular Service WARFARIN (COUMADIN) PATIENT EDUCATION What is Warfarin (Coumadin)?
Warfarin (Coumadin) is a medication that works as an anticoagulant. Anti means against ; coagulant means "blood clotting". An anticoagulant helps to prevent clots from forming in the blood. Because it decreases clotting of blood, Coumadin is sometimes called a blood-thinner. Why am I taking Warfarin? Your doctor has prescribed warfarin to prevent the formation of harmful clots or to treat an existing clot. Blood clots may form in veins, arteries, or even within the chambers of the hear. Blood clots can block blood vessels and cut off the blood supply to a portion of the body. Blood clots can also break into fragments called emboli, and be swept by the blood to other parts of the body. Emboli from veins can travel through the heart and to the lung, causing a pulmonary embolus. Emboli from the heart or arteries can travel to the brain and cause a stroke. Conditions for which physicians may recommend taking warfarin include; Atrial fibrillation Stroke Heart attack Treatment or prevention of DVT (deep vein thrombosis) or PE (pulmonary embolism) Heart valve disease Heart valve replacements How much warfarin do I take? The amount of warfarin needed varies greatly among individuals. Your bodys response to warfarin is monitored by a blood test called the Prothrombin Time (PT) or International Normalized Ratio (INR). Your warfarin dose is adjusted based on the results of these blood tests to achieve your goal range (therapeutic range) for the INR or PT. The goal range can vary depending upon the medical condition being treated. What is the PT and INR? Prothrombin Time (PT) is measured in seconds and is the time it takes for your blood to form a clot. International Normalized Ratio (INR) is a more consistent way of reporting the PT and is widely used to monitor warfarin. Your goal INR is based on your indication for warfarin. Most people have an INR of about 1.0 before they take warfarin. After they start warfarin their goal INR range is between 2.0 and 3.0, or may even be higher if you are at greater risk of forming clots. In general, if your INR is below your target range (less than 2.0), you are greater risk of forming clots and if your INR is above your target range (greater than 3.0), you are at greater risk of having bleeding complications. When do I get my blood tested? When you first start taking warfarin, you may need to get your blood tested twice each week. As your results become more consistent and your warfarin dose becomes stable, the frequency may decrease to just once a month. The frequency of your INR tests will be determined by the anticoagulation clinic staff. It is very important that you get your blood tested on the date and time that you are instructed. If you are unable to make a scheduled appointment, it is your responsibility to call and reschedule. Close monitoring
of your INR is necessary to prevent blood clots and bleeding complications associated with your warfarin therapy. What are the side effects of warfarin? Side effects with warfarin therapy are not common. Most side effects relate to the mechanism action of the warfarin; an increase in bleeding risk. Very minor bleeding may occur even when your INR is in your goal range. This may include an increase in small bruises, or slight gum bleeding when brushing your teeth. Rarely, some people experience skin rash or loss of hair when taking warfarin. If you are experiencing something abnormal that you feel may be caused by your warfarin, please contact the anticoagulation clinic. What are the signs of too much warfarin or a high INR? Minor Bleeding Easy bruising Gum bleeding while brushing teeth Nosebleed Prolonged bleeding after minor cuts Prolonged menstrual bleeding You might notice any of the above symptoms from time to time. If you are unsure whether bleeding is significant and represents a problem, it is best to call the anticoagulation clinic and report it. It may be necessary to have your INR checked to be sure that the level of blood thinning is in the desired goal range. Major Bleeding Red or dark brown urine Red or black, tarry stool Vomiting or coughing up blood Severe headache or stomachache Unexplained bruising, frequent nose-bleeds, bleeding gums, or unusual bleeding Any bleeding that is continuous or is of an excessive amount If you have a serious fall or if you hit your head, major bleeding may occur If you experience any of these signs or symptoms, contact the anticoagulation clinic, call your physician, or go to the nearest hospital emergency department immediately. What are the symptoms of too little warfarin or a low INR? Blood clotting Call your physician immediately if you notice any of the following signs and symptoms of a blood clot: Sudden weakness in any limb Numbness or tingling anywhere Visual changes or loss of sight in either eye Sudden onset of slurred speech or inability to speak Dizziness or faintness New pain, swelling, redness or heat in an extremity New shortness of breath or chest pain All of the above signs and symptoms can be serious. Remember: Call your physician immediately if any of them occur.
Page 2
When do I take my warfarin? Warfarin is taken once each day. It is important to take your warfarin at approximately the same time each day, usually in the evening. If you have difficulty remembering to take warfarin in the evening, please discuss this with the anticoagulation clinic staff. You may take warfarin with or without food. It should not upset your stomach. You may also take warfarin at the same time as most other medications. We recommend using a mediset or daily pill box to help you keep track of doses. This can be filled each week with your appropriate dose. If possible, have someone else check you after you fill the pill box. May I take generic warfarin or is the brand name Coumadin better? Generic warfarin should be just as effective as the brand name product, called Coumadin. Occasionally, a person's INR may change when they switch from one product to the other. For this reason, we ask that you continuously take either the same generic or the same brand name product and not switch back and forth. If you decide to switch, please notify us as soon as possible. It is also important for you to realize that the generic and brand name products look different. Accidents have occurred where patients were taking both the brand name and the generic (usually prescribed by two different practitioners) by mistake because they looked like two different medications! Make sure that you are not taking both, because this would be the same as doubling your warfarin dose! What do I do if I miss a dose? Try not to miss a dose of your warfarin therapy. If you do miss a dose and you remember the same day, you may take your warfarin later than the scheduled time. If it is already the next day, please call the anticoagulation clinic for further instruction. If it is a weekend or holiday and you are unable to reach us, simply skip the missed dose and resume your normal dose the next day; it is best not to double your dose in order to catch-up. Be sure to mark the missed dose on your calendar and remember to repor t it at your next anticoagulation visit. Are there drug interactions with warfarin? Warfarin interacts with many other medications. This includes prescription medication, as well as overthe-counter medication, herbs, and vitamin supplements. Therefore, it is extremely important that you contact the anticoagulation clinic whenever you start or stop any medication, herb, or vitamin. Please check with us even if the medication was prescribed by your physician! The anticoagulation clinic may order more frequent INR checks whenever a potential drug interaction occurs with your warfarin therapy. There are certain medications that you should not take with warfarin, without the knowledge of the doctor or clinic which manages your Coumadin, because these medications may decrease the bloods ability to form clots, which increases your risk of bleeding. Important points: Never take aspirin without our knowledge. If your doctor has recommended that you take one aspirin daily, your Daily dose should not exceed 325mg. Do not take any products containing aspirin (Excedrin, Alka-Seltzer, Ascription, Bayer, Bufferin, Ecotrin, Empirin, Nyquil, and Pepto Bismol) without our knowledge. Do not take ibuprofen (Advil, Motrin, Nuprin, Medipren, Excedrin IB, Haltran, Midol 200, Pamprin-IB, naproxen (Aleve, Naprosyn, and Anaprox), ketoprofen (Orudis), cimetidine (Tagamet HB), or famotidine (Pepcid AC) without our knowledge. If you need a medication for mild pain relief, we recommend using acetaminophen (Tylenol). Limit your use of acetaminophen to no more than 2 grams per day (six of the 325mg tablets or four of the 500 mg tablets).
Page 3
Is it safe to drink alcohol while taking warfarin? Alcoholic beverages, in moderation, are safe while taking warfarin. This means no more than one or two drinks on a special occasion (1 beer = 1 glass of wine = 1 cocktail/shot), and no more than one drink per day chronically. Drinking in excess of this can put you at risk of injury, as well as elevate your INR significantly and increase your risk of bleeding. Must I limit activities while taking warfarin? Since warfarin increases your risk of bleeding, we recommend avoiding activities that place you at risk of injury. You should discuss with the anticoagulation clinic staff or your physician any of your current activities and whether or not you should continue these while taking warfarin. Physical activities that are usually safe, such as walking, jogging, swimming, and gardening, may be continued. It is important to let the clinic staff know about any significant changes in activity level. Do I need to change my diet? Foods that are high in vitamin K may counteract and decrease the effect of your warfarin. Foods that are high in vitamin K are usually leafy green vegetables such as spinach and broccoli. We generally recommend no more than one serving per day of food that is high in vitamin K. However, if you consume more than this on a daily basis, we may be able to adjust your warfarin dose around your dietary intake. The most important thing to remember about your diet is to be as consistent as possible and not to binge on foods that are high in vitamin K. If you are planning on changing your diet permanently, simply call us at the anticoagulation clinic and we can monitor your INR more closely. What if I get sick? Acute illness will change your bodys response to warfarin. An episode of congestive heart failure, fever (over 101F), flu, viral/bacterial infection, nausea, vomiting or diarrhea can cause your INR to go up dramatically. If you experience any of the above, please contact us so that we can discuss how to manage your warfarin therapy. Please remember to call us before you begin taking antibiotics, or soon after you start them. Who should know that I'm taking warfarin? It is very important to tell each physician or health care provider you visit, your dentist, and each pharmacy where you have prescriptions filled that you are taking warfarin. It may affect how they will care for you in certain situations. If you are going to be taking warfarin for a long period of time, consider wearing an identification bracelet or necklace that will alert emergency health care providers that you are on warfarin. What about pregnancy? You should not take warfarin if you are pregnant. There are other, safer options for anticoagulation in women who are pregnant. Talk to your physician if you are planning on becoming pregnant so that you may be switched to another medication in time to prevent harm to the developing fetus.
Page 4
Important points to remember: Take your warfarin as directed, at the same time each day. Look for signs of bleeding or clotting and report them immediately. Notify us of any changes to your dietary vitamin K intake, activity level, or medications (including herbal products, vitamins, over-the-counter medication). Call us if you have a fever, diarrhea, vomiting, or loss of appetite lasting longer than one day. Limit alcohol to 1-2 drinks per day. Tell each of your health care providers that you are taking warfarin, carry a wallet card, and consider getting an ID bracelet or necklace. Keep all appointments or call promptly to reschedule. Call with any questions concerning your warfarin therapy!
Michael Pecora, M.D.
Page 5
También podría gustarte
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Epilepsy 2015 A Practical Guide PDFDocumento283 páginasEpilepsy 2015 A Practical Guide PDFrahma100% (1)
- Facial Wound Assessment KitDocumento9 páginasFacial Wound Assessment KitIJAR JOURNALAún no hay calificaciones
- 10.1007@s00405 020 06193 3Documento6 páginas10.1007@s00405 020 06193 3Anne SerneoAún no hay calificaciones
- Bipolar DisordersDocumento63 páginasBipolar DisorderselvinegunawanAún no hay calificaciones
- Mera MerckDocumento5 páginasMera Merckkuch bhi100% (1)
- A 3 Table of Surgical Procedures TOSP With Minor Surgical Procedures MSPs 1Documento94 páginasA 3 Table of Surgical Procedures TOSP With Minor Surgical Procedures MSPs 1Chee Yung NgAún no hay calificaciones
- PDF Fillable Medical CertDocumento4 páginasPDF Fillable Medical CertCasey PetersonAún no hay calificaciones
- Medical Device PackagingDocumento17 páginasMedical Device Packaging049 Nishigandha NadavadeAún no hay calificaciones
- Myopia APDF PDFDocumento14 páginasMyopia APDF PDFRao Sab100% (1)
- Santos, Ivan Jamil S. NCM 112-Or Rle Fear (Pre-Op) Assessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveDocumento1 páginaSantos, Ivan Jamil S. NCM 112-Or Rle Fear (Pre-Op) Assessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveIvan SantosAún no hay calificaciones
- Water Quality at Residential and Industrial AreaDocumento11 páginasWater Quality at Residential and Industrial AreaMohamad AizanAún no hay calificaciones
- Contoh IjapDocumento4 páginasContoh IjapFarihaAún no hay calificaciones
- Modern ReflexologyDocumento15 páginasModern ReflexologyusmanAún no hay calificaciones
- Internet Addiction and Its Cognitive Behavioral Therapy: Ömer Şenormancı, Ramazan Konkan and Mehmet Zihni SungurDocumento21 páginasInternet Addiction and Its Cognitive Behavioral Therapy: Ömer Şenormancı, Ramazan Konkan and Mehmet Zihni SungurShari' Si WahyuAún no hay calificaciones
- Hiv 101Documento33 páginasHiv 101Hend Al-RamahiAún no hay calificaciones
- Sample Concept MapDocumento1 páginaSample Concept MapAndrea SolumAún no hay calificaciones
- Organochlorine Compouds ToxicityDocumento39 páginasOrganochlorine Compouds ToxicityAdarshBijapurAún no hay calificaciones
- Litalatur Review HalusinasiDocumento9 páginasLitalatur Review HalusinasirehabAún no hay calificaciones
- Management of Failed Block - Harsh.Documento48 páginasManagement of Failed Block - Harsh.Faeiz KhanAún no hay calificaciones
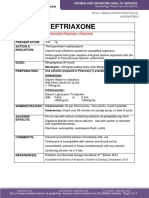
- Ceftriaxone PDFDocumento1 páginaCeftriaxone PDFveniAún no hay calificaciones
- I-STAT Hospital Navigator BrochureDocumento19 páginasI-STAT Hospital Navigator BrochureClaudia SotoAún no hay calificaciones
- Crisis CounsellingDocumento28 páginasCrisis CounsellingPooja varmaAún no hay calificaciones
- Philippine Oncology Nurses Association Registration: Basic Chemotherapy CourseDocumento2 páginasPhilippine Oncology Nurses Association Registration: Basic Chemotherapy CourseFret Ramirez Coronia RNAún no hay calificaciones
- Benefits Summary PhilippinesDocumento2 páginasBenefits Summary PhilippinesRose GeeAún no hay calificaciones
- Gestalt Sept2019 FINALDocumento3 páginasGestalt Sept2019 FINALMolly ChristensenAún no hay calificaciones
- Lista de Lucrari Buga Ana MariaDocumento4 páginasLista de Lucrari Buga Ana MarialeoAún no hay calificaciones
- Malaprabha Biogas Plant Developed by DR S V MapuskarDocumento40 páginasMalaprabha Biogas Plant Developed by DR S V Mapuskarsvmapuskar4914100% (3)
- Rehydration, Hangover and Vitamin TherapyDocumento2 páginasRehydration, Hangover and Vitamin TherapyKadek SeptiawanAún no hay calificaciones
- Thyroid Carcinoma Case PreDocumento22 páginasThyroid Carcinoma Case PreTabrrett Bethel100% (1)
- Movement Diagrams - Rayner & Smale PDFDocumento6 páginasMovement Diagrams - Rayner & Smale PDFItai IzhakAún no hay calificaciones