Documentos de Académico
Documentos de Profesional
Documentos de Cultura
How Bacteria Could Cause Cancer
Cargado por
USMP FN ARCHIVOSDescripción original:
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
How Bacteria Could Cause Cancer
Cargado por
USMP FN ARCHIVOSCopyright:
Formatos disponibles
How bacteria could cause cncer
Helicobacter pylori highlighted the potential for bacteria to cause cancer. It is becoming clear that chronic infection with other bacteria, notably Salmonella typhi, can also facilitate tumour development. Infections caused by several bacteria (e.g.Bartonella spp., Lawsonia intracellularis andCitrobacter rodentium) can induce cellular proliferation that can be reversed by antibiotic treatment. Other chronic bacterial infections have the effect of blocking apoptosis. However, the underlying cellular mechanisms are far from clear. Conversely, several bacterial toxins interfere with cellular signalling mechanisms in a way that is characteristic of tumour promoters. These include Pasteurella multocida toxin, which uniquely acts as a mitogen, and Escherichia coli cytotoxic necrotizing factor, which activates Rho family signalling. This leads to activation of COX2, which is involved in several stages of tumour development, including inhibition of apoptosis. Such toxins could provide valuable models for bacterial involvement in cancer, but more significantly they could play a direct role in cancer causation and progression. The discoveries in medical microbiology that were made towards the end of the 19th century showed how bacteria were the cause of some of the major diseases of the time and so allowed progress to be made towards improved treatment and survival. Perhaps not surprisingly, this led some to suggest that bacteria were implicated in all diseases and so at this time the idea that bacterial infections might lead to cancer was born. This proposition has had an uneasy and controversial history, which has evolved with our greater understanding of tumourigenic and infectious processes. The early observations that certain bacteria were present at the site of carcinomas did not take account of the long time-lag between initiation of the carcinogenic process and the onset of overt disease. Thus, the presence of bacteria at the site of a tumour does not in itself imply causation, in the same way that bacterial infection in cystic fibrosis patients would not be thought of as the basis of that disease. Conversely, the initial cell transformation event can occur many years before the manifestation of cancer and so an infection could be cleared long before its full consequences were seen. The role of viruses such as hepatitis B virus (HBV), Epstein Barr virus (EBV) and human papilloma virus (HPV) in carcinogenesis is accepted because of the direct mechanistic effects of often single genes that result in cell transformation [1]. The involvement of bacteria in carcinogenesis remains controversial partly because there is no clear agreement on the molecular mechanism(s) by which they might promote the development of cancer. Carcinogenesis is a protracted, multistage process that can take decades to reach its culmination (Box 1). Initially, mutations arise that release the cells from normal growth-control mechanisms, and then the transformed cells must proliferate while avoiding destruction by the immune system. Once a small tumour or focus has developed, it must be supplied with blood to allow its further growth (angiogenesis) and then dramatic changes in cell behaviour are required to permit metastatic invasin of other sites in the body. There is increasing evidence that pathogenic bacteria can contribute to specific stages in cancer development, particularly in chronic infections where, for the duration of the infection, normal cell processes can come under the influence of factors released by the pathogen. The proposition that bacterial infection could cause cancer acquired widespread interest with the revelation that Helicobacter pylori was able to establish chronic infections in the stomach. Infection was linked first to stomach ulcers then subsequently to some gastric carcinomas [2] and mucosa-associated lymphoid tissue (MALT) lymphomas [3]. Even though the precise mechanisms remain uncertain, it is becoming clear that H. pylori and several other bacteria and their products have properties that might contribute to different stages of tumour initiation and progression (Box 2). In this review, we outline ways that bacteria could promote cancer both for bacteria that are known to be involved in carcinogenesis and also for those where there is no known link, but where the effect of the bacterium on the host suggests that such a link could exist. Epidemiology of bacterial infection and carcinogenesis The relationship between H. pylori and carcinogenesis is not straightforward [4,5]. Much of the evidence to link H. pylori with carcinognesis is epidemiological and thus open to different interpretations. This is further complicated by the diversity of H. pylori isolates, which mutate and evolve within an individual such that any one person is infected with several H. pylori quasispecies, each having a different virulence potential. Consequently, it is difficult to determine which virulence factors are important in disease. Human genetic diversity is a further complicating factor, reflecting different susceptibilities to H. pylori infection and gastric cancer development [6]. In other diseases, animal models have provided convincing evidence for disease causation. Much effort has been expended in trying to set up a relevant animal model infection system for H. pylori, but the pathology displayed is often different from that seen in the human infection. There are two types of animal model: those using H. pylori in a variety of animal hosts and those using related Helicobacter species [7]. H. pylori infection of the Mongolian gerbil has conclusively been shown to induce gastric adenocarcinoma [8] and this model infection system approximates reasonably well to the human disease [9]. Several non-H. pylori models have been described, most notably Helicobacter mustelae infection in ferrets and Helicobacter felis infection in mice [4,7]. H. felis, which has been widely used to examine the link between inflammation and Helicobacter-induced carcinogenesis, differs from H. pylori in that it does not express either the
vacA gene or the cag pathogenicity island (PAI). Strains that express cagA are most often associated with gastric cancer [10,11], although cagA is only one of several genes encoded by the cag PAI that would be expected to encode related functions. Nevertheless, MALT lymphoma can be induced by H. mustelae in ferrets [12] and by H. felis in mice, where it can be treated by antimicrobial therapy [13,14]. Transgenic mouse models have also been useful in exploring the importance of H. pylori binding to human receptors [5]. Although most attention has focused on H. pylori, other bacterial infections have been known for some time to have a link with cancer. Perhaps the strongest epidemiological case is for Salmonella enterica serovar Typhi (S. typhi), the agent of typhoid, which can also lead to chronic bacterial carriage in the gallbladder. A case-control study compared those who experienced acute infection with those who subsequently became chronic carriers following the 1922 typhoid outbreak in New York. Those who became carriers were six times more likely to die of hepatobiliary carcinoma than matched controls [15]. More recent work analysing the 1964 typhoid outbreak in Aberdeen [16,17] has also suggested a strong association between chronic carrier status and hepatobiliary carcinoma and, in addition, a weaker linkage with cancer at other sites. People who contracted typhoid but who did not become carriers were not at higher risk of cancer. A similar linkage was found between S. typhi carriage and gallbladder carcinoma in Northern India, where both conditions have a high incidence [18,19]. The molecular process by which chronic S. typhi carriage promotes cancer development has yet to be determined. However, it has been suggested that the degradation of bile salts by enteric bacteria to yield carcinogenic compounds could contribute to carcinogenesis [20]. A further example of linkage between bacterial infection and carcinogenesis is provided by Citrobacter rodentium infection in mice, which causes a colonic hyperplastic disease that can lead to colonic cancer [21,22]. Immunological mechanisms involved in the induction of carcinognesis Although the linkage between H. pylori infection and gastric cancer is convincing, the molecular mechanism or mechanisms responsible are unclear, and both bacterial and host factors are implicated. One view is that increased inflammation generates reactive oxygen and nitrogen intermediates that might lead directly to DNA damage [23,24]. The role of the immune response, in particular a CD4T cell response, is supported by work using H. felis infection in mice, although it is noteworthy that polymorphonuclear lymphocyte infiltration is not a feature of this model, unlike H. pylori infection in humans [25,26]. H. pylori infection also upregulates signalling molecules; more specifically, the activation of the extracellularly regulated tyrosine kinase (ERK) signalling pathway results in an increase in important transcription factors such as activator protein 1 (AP-1) and serum response factor (SRF), which might be responsible for the upregulation of pro-inflammatory cytokines seen in H. pylori infection [27]. Inflammation is not always a feature of bacterial infections associated with proliferative lesions. Hyperplasia owing to C. rodentium infection is sometimes but not always accompanied by inflammation [28]. Lawsonia intracellularis infection has not been associated with carcinogenesis, but induces hyperproliferation with a minimal inflammatory response [29]. Similarly, Pasteurella multocida infections induce hyperproliferation without evidence of any immune response [30]. Proliferative infections It is known that protracted growth stimulation can promote tumour formation by facilitating the acquisition of mutations in genes encoding the signalling and cell cycle proteins that control proliferation. Several bacterial infections promote cell proliferation and so could increase the rate of cell transformation. H. pylori activates several genes known to be associated with carcinogenesis, such as cyclooxygenase 2 (COX2) [31], c-Jun amino-terminal kinase (JNK) [27] and phospholipase A2 [32]. The expression of cagE by H. pylori promotes activation of the cell cycle regulatory molecule cyclin D1 in a mitogen-activated protein kinase (MAPK)- dependent manner [33]. Overexpression of cyclin D1 has recently been linked with poor prognosis in cancers of several organs, including the colon and lung [34,35]. Alternatively, it has been noted that attachment of H. pylori to cells can lead to the production of autoantibodies against Lewis carbohydrate epitopes on the surface of acidproducing parietal cells [36]. This results in loss of the parietal cells and the subsequent hyperproliferation of gastric stem cells produces an adenomatous lesion. Bartonella spp. are emerging pathogens that can cause conditions, such as trench fever, Carrions disease and catscratch disease, which are characterized by the development of proliferative lesions. Bartonella bacilliformis [37] enters the bloodstream through a wound inflicted by an infected sandfly and, uniquely, colonizes circulating erythrocytes, resulting in a persistent infection that culminates in a potentially fatal haemolytic anaemia [38]. B. bacilliformis and other Bartonella spp. Can also enter endothelial cells by a RhoA-dependent invasion process with concurrent stimulation of the focal adhesion complex and the formation of actin stress fibres [39]. The infected cells acquire an abnormal morphology and tumour-like structures develop that contain fine blood capillaries. These regress following the eradication of the bacteria with antibiotics [40]. B. henselae pili promote the production of vascular endothelial growth factor (VEGF), although endothelial cell proliferation appears to be independent of direct contact between the bacterium and the host cells [41,42]. VEGF is a potent mitogen and stimulator of tumour angiogenesis and its induction by Bartonella spp. Could therefore have important consequences in terms of tumour initiation and progression, although it is currently not suggested that Bartonella infections are tumourigenic (See the Opinion article by Volkhard Kempf et al. in this issue for a discussion of the molecular mechanisms involved in Bartonella-induced
endothelial cell proliferation). L. intracellularis is the aetiological agent of proliferative enteropathy (PE) of pigs and other animal species [29]. The pathogen enters mitotic and partially differentiated cells in the tubular crypts of the intestinal epithelium and promotes their proliferation. These cells enlarge the crypts and replace the mature, differentiated enterocytes of the epithelium, giving rise to distinctive disease lesions. The lesions resemble those seen in human proliferative bowel disorders, such as Crohns disease and ulcerative colitis, that are associated with an increased risk of colorectal cancer [43]. The L. intracellularis lesions are also similar to murine colonic hyperplasia caused by C. rodentium, which it is known can accelerate the formation of colon adenomas in mice that have been treated with a chemical carcinogen [21]. C. rodentium can also initiate adenoma formation in mice defective in the Apc tumour suppressor gene [22]. This is one of the most convincing pieces of evidence that a bacterial pathogen can promote the initiation of cancer through cell transformation. Although the precise molecular events by which tumourigenesis occurs have still to be established, the 35-kb PAI encoding the locus for enterocyte effacement has been implicated [28]. Interestingly, this PAI is shared with some enteropathogenic and enterohaemorrhagic E. coli (EPEC and EHEC, respectively). The molecular mechanisms associated with these examples have not been identified. Conversely, some bacterial toxins are known to modulate intracelular signalling pathways directly in a way that could promote tumour development, although their carcinogenic potential is only now beginning to be explored. P. multocida toxin (PMT) is a potent mitogen for quiescent cells and additionally can overcome contact inhibition and is a strong inducer of anchorage-independent growth [30]. The target molecule for PMT is unknown but the toxin acts intracellularly to stimulate several signalling cascades mediated by protooncogenes including those linked to phospholipase C, protein kinase C and calcium mobilization. The subsequent activation of the ERK-1 and -2 MAPKs stimulates the cells to undergo DNA synthesis and proliferation. PMT activation of tissue culture cells also promotes RhoA-mediated signal transduction events that result in activation of focal adhesin kinase (FAK) and Src family kinases [30,44]. The activation level of these proteins is often greatly increased in many cancers and contributes to cell transformation. Experimental infection with P. multocida or injection of PMT is known to cause cell proliferation at distal sites, including the epithelium of the bladder and ureter, without evidence of inflammation [45]. Toxigenic P. multocida are principally associated with a pig nasal infection that leads to bone loss, although they have also been isolated from the sites of human wound infection and chronic respiratory carriage [46]. The protracted, mitogenic stimulation during the course of such infections could contribute towards tumour development although an epidemiological investigation has yet to be carried out. Another toxin that displays a proliferative role is epidermal differentiation-inhibiting factor (EDIN), which is expressed by some strains of Staphylococcus aureus. Subcutaneous injection of EDIN, a toxin that modifies Rho proteins, induces transient hyperplasia [47]. The suppression of apoptosis An important mechanism by which transformed cells can normally be prevented from proliferating and developing into tumours is through the induction of pre-programmed cell death or apoptosis (Fig. 1). Apoptosis results from several different extracelular stimuli but, in the case of potential cancer cells, the release of the serine protease granzyme B and tumour necrosis factor (TNF-) from activated CD8+ T cells are important mechanisms. Tumour cells can have abnormal expression levels of factors such as Bcl-2 family proteins that slow the progression of apoptosis and elevated nuclear factor (NF)-B-regulated transcription, which can inhibit TNF--induced apoptosis [48]. Several pathogenic bacteria, particularly those that can establish a persistent, intracellular infection, can suppress apoptosis in host cells. This strategy provides a niche in which an intracellular pathogen can survive in spite of the attempts of the host immune system to destroy the infected cell by inducing apoptosis. As a consequence, the suppression of apoptosis by a pathogen might also allow a partially transformed cell to evade the self-destructive process and so progress to a higher level of transformation and ultimately become tumourigenic. Mycoplasmas, which can cause chronic asymptomatic infections, can promote cell transformation and block apoptosis. Prolonged in vitro infection of tissue culture cells with Mycoplasma spp. led to cell transformation and tumourigenicity in mice, accompanied by enhanced expression of the H-ras and c-myc oncogenes [49,50]. Mycoplasma infection, or lipidassociated membrane proteins extracted from mycoplasmas, inhibits apoptosis in an NF-B-dependent manner. The enzyme COX2 is activated by H. pylori. It has recently been shown that localized overexpression of COX2 in the mammary glands of transgenic mice causes the development of tumours through the overexpression of Bcl-2 and suppression of apoptosis [51]. COX2 regulates the rate-limiting step in prostaglandin biosynthesis and is involved in physiological processes such as pain transmission, cell cycle regulation and the inflammatory response. COX2 is overexpressed in cancers of many organs although its role in colorectal cancer has been most extensively investigated. Here, the overexpression of COX2 has been linked to tumour invasiveness, which can be reduced using non-steroidal antiinflammatory drugs (NSAIDs) that inhibit the enzymatic activity of COX2 [52]. COX2 induction has been detected in gastric mucosal cells treated with lysates extracted from H. pylori. This induction is reduced in isogenic mutants of picA and picB, H. pylori virulence determinants that induce cytokine production in the gastric mucosa [31]. Because infection with H. pylori can last for a period of years, the consequent chronic induction of COX2 during the course of these infections could allow the survival of transformed cells that would otherwise become apoptotic and
die. Cytotoxic necrotizing factor (CNF), a toxin found in many uropathogenic E. coli, induces elevated expression of COX2 in murine fibroblasts [53], and is the first toxin shown to affect COX2 expression. CNF-expressing E. coli establish a persistent, intracellular infection of the urogenital tract [54] and CNF itself can suppress apoptosis by affecting the transcription levels of the Bcl-2 family proteins [55]. The suppression of apoptosis by this toxin presumably enhances the survival of cells occupied by the pathogen to facilitate a chronic infection and could be a consequence of COX2 induction. There is also a strong correlation between CNF-positive E. coli and prostatitis, and experimental prostate infections show that expression of CNF is linked to a greater inflammatory response, leading to the suggestion that CNF might contribute to prostate cancer [56]. Bacterial toxins and Rho protein activation The Rho family of small GTPases act as key molecular switches that integrate signals from several different signal transduction pathways. These also control and regulate movement and other aspects of cytoskeletal changes. It is becoming clear that these proteins can play a key role in carcinogenesis [57], either through their aberrant activation, which can result in uncontrolled proliferation and growth transformation, or by regulating processes downstream of other oncogenes such as Ras. Indeed, RhoC has recently been implicated as a marker for highly angiogenic and aggressive breast cancer with a high metastatic ability [58]. Interestingly, the Rho proteins are targets for several bacterial toxins, some of which have already been discussed, that can promote or inhibit their activation [59]. Transient activation of Rho proteins, particularly RhoA, often occurs during bacterial attachment to a host cell or during internalization, for example in the case of Bartonella spp. invading endothelial cells [31]. The development of stress fibres and focal adhesion signalling complexes indicative of RhoA activation is also observed in cells treated with PMT [30], but two bacterial toxins the dermonecrotic toxin of Bordetella spp. and CNF each act directly on Rho family proteins to bring about their irreversible activation [59]. CNF constitutively activates RhoA, Rac1 and Cdc42 to stimulate dramatic cytological effects through the rearrangement of actin filaments. The action of CNF on the Rho proteins also leads to perturbation of the cell cycle by inducing DNA synthesis while inhibiting cytokinesis and also modulates the activity of factors that affect apoptosis as we have indicated. As CNF-expressing E. coli establish chronic infections, the protracted stimulation of Rho protein-regulated signalling pathways during the course of the infection could have a role in carcinogenesis. Conversely, EDIN and related toxins from Bacillus cereus and Clostridium spp. Modify a subset of Rho family proteins to inactivate them, whereas another group of toxins inactivate all members of the Rho family [59]. Although it is known that EDIN can induce hyperplasia, the potential proliferative effects of this latter group of toxins has not been investigated. Conclusion The number of examples where epidemiological evidence has linked prior and chronic bacterial infection to tumour formation is growing, but the molecular mechanisms involved remain far from clear. For example, despite much research, it remains uncertain which of the many virulence factors produced by H. pylori have most significance for cancer development. Conversely, several bacteria and their products have properties that could advance carcinogenesis although there is currently no known link between these bacteria and tumour formation. Many pathogenic bacteria subvert host cell signalling pathways and so control cell behaviour to enhance survival of the pathogen. The regulation of these signalling factors is central to the development or inhibition of tumour formation. Perturbation of host signalling appears to be a particular feature of chronic infection with intracellular bacteria, in that chronic bacterial infection requires that infected cells proliferate and are resistant to the normal control mechanisms. Such infections can mimic some of the gross effects seen in tumourigenesis, and indeed the pseudocancerous lesions formed in such infections can regress with antibiotic treatment and clearance of the bacteria. A more generally applicable conclusion is that chronic infection with bacteria that perturb cell signalling processes is highly likely to contribute to cell transformation by facilitating an anti-apoptotic, proliferative state that encourages tumour initiation and promotion. Greater understanding of the consequences of long-term infections and the mechanisms that allow this balance between the host and the pathogen to be maintained will allow us to state with certainty to what extent and by which mechanisms bacteria cause cancer. Box 1. The development of cncer Cancers arise from the transformation of a single cell so that its behaviour is no longer under the control of normal regulatory pathways (Fig. I). Such uncontrolled cells behave as distinct organisms and subpopulations arise from these cells, which develop in a manner that is detrimental to the parent organism. Each stage in tumour development requires mutations in additional genes so that the development of cancer is the product of a small number of mutations accumulated over a long time period and subjected to selection. Initiation depends upon the acquisition of an oncogene from an invading virus or the mutation of a cellular protooncogene so that it is expressed abnormally. The probability of such a mutation occurring is greatly increased under conditions of protracted stimulation of cell division through chronic inflammation or tissue damage. The transformed cell proliferates in situ, unchecked by its own apoptotic pathway and avoiding the surveillance of the immune system to form a small focus. The developing tumour must redirect
the bodys blood supply to continue its growth beyond a very limited size. This process of angiogenesis requires the abnormal expression of genes, particularly growth factors such as vascular endothelial growth factor (VEGF), to promote the growth of capillaries from nearby blood vessels. After time a subset of the cells in a tumour acquire mutations in genes that regulate cell-to-cell adhesion and migration although adhesion to the extracellular matrix. These cells continue to proliferate and mutate and either migrate or are carried by the circulatory system to other parts of the body where they develop into secondary tumours. These invading cells cause major disruption to crucial physiological processes often at sites distant from that of initiation, the consequences of which are often fatal. Fig.I. The different stages involved in tumour development.
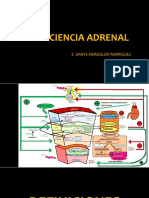
Box 2. Bacterial involvement in tumour development Schematic diagram showing how bacterial interference with cell signalling can contribute to tumour development (Fig. I). It is becoming clear that many bacterial infections rely upon precise interactions between the pathogen and components of the regulatory systems of the host cell. As cancers arise through dysfunction of these same regulatory systems, it seems inevitable that some bacterial infections can contribute to tumour development. Infections that induce cell proliferation might increase the incidence of cell transformation and the rate of tumour development through an increased rate of genetic mutation. The stimulation of proliferation and DNA replication through activation of mitogen-activated protein kinase (MAPK) pathways and cyclin D1 occurs in several infections. Several infections, particularly those in which the pathogen becomes intracellular, are associated with the suppression of apoptosis often through modulation of the expression of Bcl-2 family proteins. Another mechanism for suppressing apoptosis could be through Ras-mediated activation of cyclin-dependent kinases to overcome the tumour suppressive effects of the retinoblastoma protein Rb. By blocking apoptosis, bacterial infection could allow partially transformed cells to escape destruction and progress to a higher level of transformation, ultimately resulting in tumourigenesis. Angiogenesis is an important feature of tumour growth. The growth of blood capillaries is observed in the pseudo-tumours induced by Bartonella spp. The signalling molecules associated with cell adhesion particularly those linked to the focal adhesin complex such as focal adhesion kinase (FAK) and Src are known to play a role in tumourigenesis and even to be oncogenic themselves. The assembly of focal adhesions can be regulated through the Rho family of small GTPases that are targets for many bacterial toxins. By perturbing Rho family proteins it is possible to affect many signalling pathways because of the lateral connections between the pathways, which ordinarily allow for very precise regulation of cellular responses. Rho proteins are pivotal in cellular control and the consequences of their dysregulation by bacterial toxins have yet to be fully investigated.
Fig. I. Signalling pathways targeted by bacteria and bacterial toxins. The components of signalling pathways that are known to be affected by various bacterial toxins are indicated. It should be noted that these components are not necessarily the primary targets of these toxins. For some bacteria, the specific bacterial product responsible has not been identified. Where there is a known association with cancer the bacteria are shown in blue, whereas those with no proven link to carcinogenesis are in black. It should be noted that the signalling pathways stimulated by known carcinogenic bacteria are not necessarily the mechanism by which they influence carcinogenesis. Abbreviations: CDK, cyclin-dependent kinase; CNF, cytotoxic necrotizing factor; COX, cyclooxygenase; E2F, elongation factor 2F; FAK, focal adhesion kinase; MAPK, mitogenactivated protein kinase; NF-B, nuclear factor B; PI3K, phosphatidylinositol 3 kinase; PKB, protein kinase B; Rb, retinoblastoma; TK, tyrosine kinase; VEGF, vascular endothelial growth factor. Fig. 1. Apoptosis or programmed cell death is an important process in the development of multicellular organisms and can be induced through ligands that bind to integral membrane receptors. Apoptosis also plays a role in helping to destroy infected or malignant cells and can be triggered by factors released by activated CD8+ lymphocytes and macrophages. Tumour necrosis factor (TNF-) acts through a membrane receptor (TNF-R) whose death domain (DD) interacts with a group of proteins called TNF-receptor-associated factors (TRAFs), which are differentially expressed and can regulate transcription factors such as JUN or nuclear factor (NF)B, which promote or suppress apoptosis, respectively. The activated TNF-R also complexes with the protease caspase-8 through TNF-receptor-associated death domain protein (TRAD) and Fasassociated death domain protein (FADD) to activate the caspase cascade, which results in the proteolytic degradation of proteins involved in cell adhesion, signalling and cytoskeletal regulation. Caspase-3 activates the caspase-activated DNase (CAD) nuclease, which introduces single-strand breaks into the genomic DNA resulting in activation of the p53 tumour suppressor and cell cycle arrest. Caspase-8 also proteolytically activates the Bcl-2 family protein Bid allowing it to complex to other family members such as Bax and Bak. This complex translocates to the mitocondria and promotes the release of cytochrome c into the cytoplasm, which associates with apoptotic protease-activating factor 1 (APAF-1) to activate caspase-9 and so activate the proteolytic cascade by another route. The translocation of Bid to the mitochondria is blocked when it is complexed to other Bcl-2 family proteins like Bcl-xL or Bcl-2 itself, which suppresses apoptosis. The Bcl-2 family proteins have an important role in regulating apoptosis and it is
interesting that some pathogenic bacteria can enhance the expression of anti-apoptotic members of this family, presumably to enhance intracellular survival.
También podría gustarte
- Medicina III - Insuficiencia AdrenalDocumento41 páginasMedicina III - Insuficiencia AdrenalUSMP FN ARCHIVOSAún no hay calificaciones
- (Lab) Patología II - Esófago y EstómagoDocumento82 páginas(Lab) Patología II - Esófago y EstómagoUSMP FN ARCHIVOSAún no hay calificaciones
- English Practice Passive VoiceDocumento2 páginasEnglish Practice Passive VoiceUSMP FN ARCHIVOSAún no hay calificaciones
- How Is Osteoporosis DiagnosedDocumento3 páginasHow Is Osteoporosis DiagnosedUSMP FN ARCHIVOSAún no hay calificaciones
- Reported Speech Exercises 2013 PDFDocumento13 páginasReported Speech Exercises 2013 PDFjesusjaviermartin86% (7)
- By The Early 2020sDocumento1 páginaBy The Early 2020sUSMP FN ARCHIVOSAún no hay calificaciones
- Conditionals SentencesDocumento49 páginasConditionals SentencesUSMP FN ARCHIVOS100% (5)
- Modals PracticeDocumento2 páginasModals PracticeUSMP FN ARCHIVOSAún no hay calificaciones
- Conditionals WorksheetDocumento2 páginasConditionals WorksheetUSMP FN ARCHIVOSAún no hay calificaciones
- Daily AspirinDocumento2 páginasDaily AspirinUSMP FN ARCHIVOSAún no hay calificaciones
- Passive Voice WorksheetDocumento2 páginasPassive Voice WorksheetUSMP FN ARCHIVOSAún no hay calificaciones
- PassiveDocumento20 páginasPassiveUSMP FN ARCHIVOSAún no hay calificaciones
- How Can You Relieve MigraineDocumento3 páginasHow Can You Relieve MigraineUSMP FN ARCHIVOSAún no hay calificaciones
- Future Simple WorksheetDocumento2 páginasFuture Simple WorksheetUSMP FN ARCHIVOSAún no hay calificaciones
- The New Stem Cell Biology (Something For Everyone)Documento14 páginasThe New Stem Cell Biology (Something For Everyone)USMP FN ARCHIVOSAún no hay calificaciones
- Genomic Medicine - A PrimerDocumento8 páginasGenomic Medicine - A PrimerUSMP FN ARCHIVOSAún no hay calificaciones
- Breast Cancer WorksheetDocumento2 páginasBreast Cancer WorksheetUSMP FN ARCHIVOSAún no hay calificaciones
- A Tour of The Cardiovascular SystemDocumento2 páginasA Tour of The Cardiovascular SystemUSMP FN ARCHIVOSAún no hay calificaciones
- Bases Moleculares Del CáncerDocumento15 páginasBases Moleculares Del CáncerMairim Adn-a JóasAún no hay calificaciones
- Oncogenes and CancerDocumento7 páginasOncogenes and CancerUSMP FN ARCHIVOSAún no hay calificaciones
- Inherited Diseases Involving G ProteinsDocumento6 páginasInherited Diseases Involving G ProteinsUSMP FN ARCHIVOSAún no hay calificaciones
- Diabetes WorksheetDocumento1 páginaDiabetes WorksheetUSMP FN ARCHIVOSAún no hay calificaciones
- Diabetes (En)Documento4 páginasDiabetes (En)USMP FN ARCHIVOSAún no hay calificaciones
- Breast Cancer (En)Documento7 páginasBreast Cancer (En)USMP FN ARCHIVOSAún no hay calificaciones
- LASIK (En)Documento4 páginasLASIK (En)USMP FN ARCHIVOSAún no hay calificaciones
- Reference Summary: X-Plain LasikDocumento0 páginasReference Summary: X-Plain LasikUSMP FN ARCHIVOSAún no hay calificaciones
- The Expanding Spectrum of G Protein DiseasesDocumento6 páginasThe Expanding Spectrum of G Protein DiseasesUSMP FN ARCHIVOSAún no hay calificaciones
- The Eye WorksheetDocumento3 páginasThe Eye WorksheetUSMP FN ARCHIVOS100% (2)
- Lasik TestDocumento2 páginasLasik TestUSMP FN ARCHIVOSAún no hay calificaciones
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (119)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2099)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Aircraft ChecksDocumento10 páginasAircraft ChecksAshirbad RathaAún no hay calificaciones
- Lesson 5 CMADocumento10 páginasLesson 5 CMAAssma SabriAún no hay calificaciones
- Voltaire's Candide and the Role of Free WillDocumento3 páginasVoltaire's Candide and the Role of Free WillAngy ShoogzAún no hay calificaciones
- Mechanical Questions & AnswersDocumento161 páginasMechanical Questions & AnswersTobaAún no hay calificaciones
- Dr. Malik's Farms BrochureDocumento18 páginasDr. Malik's Farms BrochureNeil AgshikarAún no hay calificaciones
- Learning Online: Veletsianos, GeorgeDocumento11 páginasLearning Online: Veletsianos, GeorgePsico XavierAún no hay calificaciones
- HP 5973 Quick ReferenceDocumento28 páginasHP 5973 Quick ReferenceDavid ruizAún no hay calificaciones
- Marksmanship: Subject: III. Definition of TermsDocumento16 páginasMarksmanship: Subject: III. Definition of TermsAmber EbayaAún no hay calificaciones
- PGP TutorialDocumento21 páginasPGP TutorialSabri AllaniAún no hay calificaciones
- The Polynesians: Task1: ReadingDocumento10 páginasThe Polynesians: Task1: ReadingHəşim MəmmədovAún no hay calificaciones
- MSC Euribia - 2023-06-01Documento2 páginasMSC Euribia - 2023-06-01蔡國懷Aún no hay calificaciones
- Lab ReportDocumento5 páginasLab ReportHugsAún no hay calificaciones
- SOP for Troubleshooting LT ACB IssuesDocumento9 páginasSOP for Troubleshooting LT ACB IssuesAkhilesh Kumar SinghAún no hay calificaciones
- Wika Type 111.11Documento2 páginasWika Type 111.11warehouse cikalongAún no hay calificaciones
- Presentation On Ich Topics & Guidelines With A Special Reference ToDocumento79 páginasPresentation On Ich Topics & Guidelines With A Special Reference ToVidyaAún no hay calificaciones
- Hotel Design Planning and DevelopmentDocumento30 páginasHotel Design Planning and DevelopmentTio Yogatma Yudha14% (7)
- Samsung 55 Inch LCD LED 8000 User ManualDocumento290 páginasSamsung 55 Inch LCD LED 8000 User ManuallakedipperAún no hay calificaciones
- The Rich Hues of Purple Murex DyeDocumento44 páginasThe Rich Hues of Purple Murex DyeYiğit KılıçAún no hay calificaciones
- CCEE SWD Basic Levers ToolDocumento28 páginasCCEE SWD Basic Levers ToolDivina Margarita Gómez AlvarengaAún no hay calificaciones
- 256267a1Documento5083 páginas256267a1Елизавета ШепелеваAún no hay calificaciones
- EMECH 2 MarksDocumento18 páginasEMECH 2 MarkspavanraneAún no hay calificaciones
- Using Snapchat For OSINT - Save Videos Without OverlaysDocumento12 páginasUsing Snapchat For OSINT - Save Videos Without OverlaysVo TinhAún no hay calificaciones
- CIGB B164 Erosion InterneDocumento163 páginasCIGB B164 Erosion InterneJonathan ColeAún no hay calificaciones
- Lec 10 - MQueues and Shared Memory PDFDocumento57 páginasLec 10 - MQueues and Shared Memory PDFUchiha ItachiAún no hay calificaciones
- Khaton Prayer BookDocumento47 páginasKhaton Prayer BookKarma TsheringAún no hay calificaciones
- Arduino Nano based K1EL Winkeyer compatible CW contest keyerDocumento35 páginasArduino Nano based K1EL Winkeyer compatible CW contest keyerSreejith SreedharanAún no hay calificaciones
- Design and Analysis of Algorithms Prof. Madhavan Mukund Chennai Mathematical Institute Week - 01 Module - 01 Lecture - 01Documento8 páginasDesign and Analysis of Algorithms Prof. Madhavan Mukund Chennai Mathematical Institute Week - 01 Module - 01 Lecture - 01SwatiAún no hay calificaciones
- Research Paper Theory of Mind 2Documento15 páginasResearch Paper Theory of Mind 2api-529331295Aún no hay calificaciones
- Compare and Contrast High School and College EssayDocumento6 páginasCompare and Contrast High School and College Essayafibkyielxfbab100% (1)
- 3.2 Probability DistributionDocumento38 páginas3.2 Probability Distributionyouservezeropurpose113Aún no hay calificaciones