Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Quiz 2
Cargado por
Gerald Resubal OriñaDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Quiz 2
Cargado por
Gerald Resubal OriñaCopyright:
Formatos disponibles
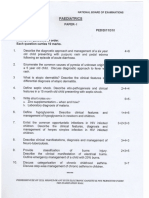
Situation 1. Mrs. Rosa, a 56 year old was admitted to a medical-surgical unit with an exacerbation of Congestive Heart Failure (CHF).
The client presents with a past medical history of an anterior wall myocardial infarction (MI), diabetes, and hypertension. The client complains of fatigue and shortness of breath. 1. Mrs. Rosa is experiencing dyspnea. Which of the following actions is the first the nurse should perform? a. Ask the patient to lie down on the exam table. b. Draw blood for chemistry panel and arterial blood gas (ABG). c. Send the patient for a chest x-ray. d. Check blood pressure. 2. The doctor ordered medications for the patient. Which of the following drug classification should the nurse question the doctor if prescribed for a person with congestive heart failure? a. Angiotensin-converting enzyme (ACE) inhibitor b. Beta-adrenergic blocker c. Alpha-adrenergic antagonist d. Thiazolidinediones 3. Upon assessing the patient with left-sided heart failure, the nurse should expect to find: a. Crushing chest pain b. Dyspnea on exertion c. Extensive peripheral edema d. Jugular vein distention 4. Which of the following questions is most important to ask in a client with congestive heart failure who has jugular vein distention? a. At what time do you go to sleep during the night? b. How many pillows do you use when lying down? c. What do you drink before going to sleep? d. How many hours of night sleep do you have? 5. Mrs. Rosa developed hyperaldosteronism secondary to congestive heart failure. The doctor ordered to start spironolactone (Aldactone) to manage the disorder. The nurse informs the patient that the need for dosage adjustment may be necessary if which of the following medications is also being taken? a. Potassium chloride c. Warfarin sodium (Coumadin) b. Alprazolam (Xanax) d. Verapamil hydrochloride (Calan) Situation 2. A 68 year old man was brought to emergency unit. He is suspected to have coronary artery disease presents with atypical chest pain and hyperlipidemia. The client has history of cigarette smoking, hypertension, and diabetes mellitus.
6. Nurse Germaine is reviewing the assessment data of the client. Which finding would be most important for the patient to modify to lessen the risk for coronary artery disease (CAD)? a. Elevated triglyceride levels b. Elevated serum lipase levels c. Elevated low-density lipoprotien(LDL) level d. Elevated high-density lipoprotein(HDL) level 7. Nurse Charisse has the knowledge of the disease if she knows that the most commonly condition resulted in coronary artery disease is: a. Atherosclerosis c. Myocardial Infarction b. Diabetes Mellitus d. Renal failure 8. When teaching a client with coronary artery disease about nutrition, Nurse Iris should emphasize one of the following; a. Eating three balanced meals a day b. Adding comlex carbohydrates c. Avoiding heavy meals d. Limiting sodium to 7gms per day 9. The patient is scheduled for a cardiac catheterization. Following the procedure, the priority nursing action is to assess the: a. Catheter insertion site c. Potassium level b. Temperature d. Urine output 10. Which of the following actions is the first priority care for a patient exhibiting signs and symptoms of coronary artery disease? a. Decrease anxiety b. Enhance myocardial oxygenation c. Administer sublingual nitroglycerin d. Educate the patient about his symptoms. Situation 3. Mr. Bean, a 63 year old man is evaluated in the emergency department for a threeday history of increasing dyspnea. She was diagnosed with severe chronic obstructive pulmonary disease (COPD) requiring long-term oxygen therapy. His baseline PCO2 is 48mmHg. He has had increasing cough but without chest pain. 11. The doctor ordered an arterial blood gases to be dawn from Mr. Bean. Which of the following is the minimum lengh of time the nurse should plan to hold pressure on the puncture site? a. 2 minutes c. 10 minutes b. 5 minutes d. 15 minutes 12. Nurse Donver is performing assessment to Mr. Bean. Which of the following findings should he expect to observe? a. Non-productive cough
b. Prolonged inspiration c. Vesicular breath sounds d. Increased anterior-posterior chest diameter 13. Mr.Bean is taking Aminophylline drug and while taking the drug, the therapeutic level must be obtained. Laboratory results indicate that the patients serum aminophylline level is 17 mcg/mL. The nurse recognizes the aminophylline level is: a. Within therapeutic range. b. Too high and should be reported. c. Questionable and should be repeated. d. Too low to be therapeutic. 14. The patient is using an ipratropium inhaler and Nurse Ricah asked him about the proper use of the device. Which of the following statements made by the patient indicates a need for futher education regarding the use of inhaler? a. I should rinse my mouth following the two puffs to get rid of bad taste. b. I should wait at least 1 to 2 minutes between each puff of the inhaler. c. If my breathing gets worse, I should keep taking extra puffs of the inhaler until I can breathe more easily. d. Because this medication is not fast-acting, I cannot use it in an emergency if my breathing gets worse. 15. Nurse Mae is preparing to estabish oxygen therapy for a patient with COPD, and the physicians prescription reads Oxygen per nasal cannula at 5L per minute. Which of the following actions should the nurse take? a. Administer the oxygen as prescribed. b. Call the physician and question the correct flow rate of the oxygen. c. Establish the oxygen as prescribed and obtain an ABG. d. Change the delivery device from a nasal cannula to a simple oxygen mask.
También podría gustarte
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- NCLEX Fluids & ElectrolytesDocumento6 páginasNCLEX Fluids & ElectrolytesNathalee Walker100% (1)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- Word Perioperative NursingDocumento19 páginasWord Perioperative NursingGerald Resubal Oriña100% (1)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- Medical-Surgical Nursing QuizDocumento3 páginasMedical-Surgical Nursing QuizGerald Resubal Oriña100% (1)
- Parkinson's DiseaseDocumento65 páginasParkinson's DiseaseGerald Resubal OriñaAún no hay calificaciones
- NCP AppendicitisDocumento8 páginasNCP AppendicitisAaron_Kim_Vela_4636Aún no hay calificaciones
- Barksy - The Paradox of Health PDFDocumento5 páginasBarksy - The Paradox of Health PDFdani_g_1987Aún no hay calificaciones
- 2001 Pharmacology McqsDocumento10 páginas2001 Pharmacology McqsKenneth MiguelAún no hay calificaciones
- NCP For Acute Gastroenteritis (Pediatric)Documento6 páginasNCP For Acute Gastroenteritis (Pediatric)abcel76% (21)
- Mothers ClassDocumento3 páginasMothers ClassGerald Resubal Oriña100% (1)
- MCQ Final 2014Documento19 páginasMCQ Final 2014JohnSon100% (1)
- Surgical Instruments 3Documento110 páginasSurgical Instruments 3Gerald Resubal OriñaAún no hay calificaciones
- Anti-Epilepsy Agents: Prepared By: Gerald R. Oriña BSN-2B Mrs. Jessica SabasDocumento32 páginasAnti-Epilepsy Agents: Prepared By: Gerald R. Oriña BSN-2B Mrs. Jessica SabasGerald Resubal OriñaAún no hay calificaciones
- Assessment Questions (Assessment Criteria)Documento2 páginasAssessment Questions (Assessment Criteria)sujanaAún no hay calificaciones
- VS TL - Protein - L1 29261 2303 3Documento7 páginasVS TL - Protein - L1 29261 2303 3Hadi BitarAún no hay calificaciones
- Osteoporosis PhilippinesDocumento3 páginasOsteoporosis PhilippinesMia DangaAún no hay calificaciones
- Paediatrics: Final Exam National Board of Examinations December 2011Documento4 páginasPaediatrics: Final Exam National Board of Examinations December 2011AlolikaAún no hay calificaciones
- 9497Documento45 páginas9497David axtonAún no hay calificaciones
- Caring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyDocumento34 páginasCaring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyRubinaAún no hay calificaciones
- Assessment Diagnosis Rationale Plan Interventions Rationale EvaluationDocumento14 páginasAssessment Diagnosis Rationale Plan Interventions Rationale EvaluationDuran JustineAún no hay calificaciones
- Itls 9th Edition Prep Packet Advanced Provider VersionDocumento19 páginasItls 9th Edition Prep Packet Advanced Provider VersionUmidagha BaghirzadaAún no hay calificaciones
- Health Assessment Made Incredibly Visual Incredibly Easy Series 2nd Edition PDFDrive 9 18Documento10 páginasHealth Assessment Made Incredibly Visual Incredibly Easy Series 2nd Edition PDFDrive 9 18mianpenarandaAún no hay calificaciones
- Case Report Two Blue Chromhidrosis Patients in Emergency RoomDocumento2 páginasCase Report Two Blue Chromhidrosis Patients in Emergency RoomInternational Journal of Innovative Science and Research TechnologyAún no hay calificaciones
- Maternal Health Research Priorities PDFDocumento9 páginasMaternal Health Research Priorities PDFIshrat PatelAún no hay calificaciones
- Hope 1 - FitnessDocumento13 páginasHope 1 - FitnessMark Clemence R. ParcasioAún no hay calificaciones
- M SDocumento162 páginasM SAnn Claudette SyAún no hay calificaciones
- 1.7 Surgery For Cyst or Abscess of The Bartholin Gland With Special Reference To The Newer OperatasDocumento3 páginas1.7 Surgery For Cyst or Abscess of The Bartholin Gland With Special Reference To The Newer OperatasMuh IkhsanAún no hay calificaciones
- 4D CT With Respiratory GatingDocumento2 páginas4D CT With Respiratory GatingLaura Karina Sanchez ColinAún no hay calificaciones
- 209 (8) 6Documento1 página209 (8) 6Rajesh DmAún no hay calificaciones
- Review Article: Inhaled Therapy in Respiratory Disease: The Complex Interplay of Pulmonary Kinetic ProcessesDocumento12 páginasReview Article: Inhaled Therapy in Respiratory Disease: The Complex Interplay of Pulmonary Kinetic ProcessesliadiafaridaAún no hay calificaciones
- WHO - HQ - Reports G2 PROD EXT TBCountryProfileDocumento1 páginaWHO - HQ - Reports G2 PROD EXT TBCountryProfileAngelo Santos EstrellaAún no hay calificaciones
- Drug Study Ceftriaxone SodiumDocumento3 páginasDrug Study Ceftriaxone SodiumPrincess Queenie OlarteAún no hay calificaciones
- Intestinal Amoebiasis CSDocumento34 páginasIntestinal Amoebiasis CSabigailxDAún no hay calificaciones
- Foreign Body AspirationDocumento4 páginasForeign Body AspirationpriscaAún no hay calificaciones
- Radiologia in Spondilita AnchilozantaDocumento18 páginasRadiologia in Spondilita AnchilozantaMarina ApostolAún no hay calificaciones
- JM Shah Benefits of BiowellDocumento2 páginasJM Shah Benefits of BiowellManagerAún no hay calificaciones
- Bowel IncontinenceDocumento4 páginasBowel IncontinenceprashanthAún no hay calificaciones