Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Chapter II Edited Jeff
Cargado por
Roderick AgbuyaDerechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Chapter II Edited Jeff
Cargado por
Roderick AgbuyaCopyright:
Formatos disponibles
CHAPTER II REVIEW OF RELATED LITERATURE This chapter presents related literature and studies which have bearing and
relevance to the problem under study. This chapter provides the necessary background carrying out the present investigation. Breast Milk According to the American Academy of Pediatrics (2007), breast milk is made from nutrients in the mother's bloodstream and bodily stores. Breast milk has just the right amount of fat, sugar, water, and protein that is needed for a baby's growth and development. Because breastfeeding uses an average of 500 calories a day, it helps the mother lose weight after giving birth. The composition of breast milk changes depending on how long the baby nurses at each session, as well as on the age of the child. The quality of a mother's breast milk may be compromised by smoking, alcoholic beverages, caffeinated drinks, marijuana, methamphetamine, heroin, and methadone. Tobacco smoking by mothers is not a contraindication to breastfeeding. In addition, the AAP states that while breastfeeding mothers should avoid the use of alcoholic beverages, an occasional celebratory single, small alcoholic drink is acceptable, but breastfeeding should be avoided for 2 hours after the drink. Lawrence (2008) pointed out that breast milk contains a unique composition of nutrition especially made for the human infant. The amount of protein changes after the childs needs, among other things it contains cholesterol and taurine that is important for
the infant. Breast milk also holds a lot of antibodies against gastrointestinal and respiratory diseases. History of Breastfeeding Nathoo, Tasnim, Ostry, and Aleck (2009) noted the history of breastfeeding. In the Egyptian, Greek and Roman empires, women usually fed only their own children. However, breastfeeding began to be seen as something too common to be done by royalty, and wet nurses were employed to breastfeed the children of the royal families. This was extended over the ages, particularly in Western Europe, where noble women often made use of wet nurses. But lower class women breastfed their infants and used a wet nurse only if they were unable to feed their own infant. Attempts were made in 15th century Europe to use cow or goat milk, but these attempts were not successful. In the 18th century, flour or cereal mixed with broth was introduced as substitutes for breastfeeding, but this did not have a favorable outcome either. During the early 1900's breastfeeding started to be viewed negatively by Western societies, especially in Canada and the USA. These societies considered it a low class and uncultured practice, viewing it with a certain degree of disgust.. This coincided with the appearance of improved infant formulas in the mid 19th century and its increased use, which accelerated after World War II. From the 1960s onwards, breastfeeding experienced a revival which continues to the 2000s, though negative attitudes towards the practice were still entrenched up to 1990s. Breastfeeding Benefits American Academy of Pediatrics (AAP) (2005), stated the compelling benefits of breastfeeding for infants, mothers, families, and our society, continue to be well
supported by increasing amounts of scientific evidence. USDHHS, Office on Womens Health ( 2006), said that infants not exclusively breastfed for six months are more likely to develop a wide range of infectious diseases including ear infections, diarrhea,
respiratory illnesses, and have more hospitalizations. Because breastfed infants typically require less sick visits, prescriptions, and hospital admissions, lower-income families can benefit greatly from the cost savings associated with breastfeeding. Lawrence (2008) study shown that children who have been exclusively breastfed, when the infant only receives breast milk and no additional food or drink, including water, for at least 4 months have a lower risk of develop allergy such as asthma and eczema. Breastfeeding also has psychological benefits for the woman and the infant and help the woman to recover after the partum. The profits of breastfeeding do not only last for as long as breastfeeding is continued. For both the mother and the child there are many long-term benefits. Lower rates of overweight and type-2 diabetes have been shown among breastfed children. Women who have breastfed have been shown to have a decreased risk of cancer in breast and ovaries (WHO, 2008). World Health Organization recommendations The World Health Organization (WHO) (2010) recommends that all infants shall breastfeed exclusively for six months and together with The United Nations Childrens Fund, UNICEF, WHO has launched Baby-friendly hospitals which are obliged to promote breastfeeding and work with Ten steps to successful breastfeeding. Ten steps to successful breastfeeding includes recommendations to healthcare givers, information to the pregnant woman and support to the post partum woman. All steps
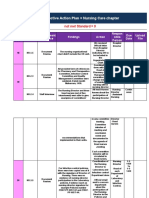
support breastfeeding as the superior infant feeding method. WHO reclaims that governments all over the world have the responsibility to protect families from formula advertising by the Intern National Code of Marketing of Breast milk Substitutes. Moreover, the governments shall see to that the women have the access to skilled support for initiating and sustaining exclusive breastfeeding for six months and healthcare professionals should be able to give effective feeding counseling. Millennium Development Goals Millennium Development Goals (MDG) (2012) highlighted that reaching the MDG on reducing child mortality will require universal coverage with key effective, affordable interventions: care for newborns and their mothers; infant and young child feeding; vaccines; prevention and case management of pneumonia, diarrhea and sepsis; malaria control; and prevention and care of HIV/AIDS. In countries with high mortality, these interventions could reduce the number of deaths by more than half. Every day approximately 940 adolescents and women worldwide die due to complications from pregnancy or childbirth. This recent data shows a decline in maternal mortality from the previously stated statistic of 1500 women dying daily, which had been considered unchanging for years. This is good news showing that priority given to sexual and reproductive health can have significant impact. However, there remain large discrepancies in maternal mortality rates throughout the world. More than 50% of the deaths occur in only six countries and the prevalence of HIV and AIDS has had a significant impact on maternal mortality rates in some countries. Adolescents aged 15 through 19 are twice as likely to die during pregnancy or child birth as those
over age 20; and girls under age 15 are five times more likely to die. Many unsafe abortions among adolescent girls, at least 2.5 million every year, are the result of unintended pregnancies and the inability to access to reproductive health information and services. Unsafe abortion significantly contributes to high rates of maternal morbidity (including short-term and long-term effects of disease, injury, impairment or disability) and mortality rates, particularly in developing countries. Adolescent Mothers Breastfeeding According to Ruth (2009), breastfeeding is a particular challenge for young mothers, who often consider breastfeeding to be too confining of their movements and too demanding of their time. So it is your task to help maintain a realistic perspective that supports the young mother in making a decision that she is comfortable with and can successfully carry out. Help her achieve her identity and minimize role confusion as she negotiates between her personal development needs and her role as a mother. One way you can do this is by emphasizing that she is the only one who can mother her baby when she breastfeeds. Offer her a different perspective; rather than seeing breastfeeding as keeping her tied down, explain that she is doing something important that no one else can take over. Emphasizing that breastfeeding is convenient and is rewarding to the mother. Provide breastfeeding guidance from the moment of delivery by giving practical suggestions to maximize the mothers success and confidence. According to Lawrence (2008), several factors have been identified as having a significant impact on a mothers decision to initiate or continue breastfeeding. These include the attitudes of healthcare providers; the mothers support network that may include fathers/partners, family members, and/or friends; hospital practices such as
providing infant formula to newborns; a mothers personal experience; and workplace environment. Mothers typically know that breastfeeding is the best way to feed their infants. However, mothers may not know about the personal health benefits associated with breastfeeding. Some mothers are challenged with combining breastfeeding and other competing demands and may focus on the barriers to breastfeeding rather than the benefits. Exploring both the benefits and barriers is an effective way to counsel a new mother. Research has shown that the common barriers to breastfeeding are embarrassment, lack of social support, lack of time, and competing demands on the mother. Embarrassment is the primary barrier for women of all backgrounds and in all regions of the country. Strategies to address embarrassment include teaching mothers how to breastfeed discretely, providing the opportunity to discuss mothers concerns, and reassuring mothers they are doing something good for their infant. Lack of social support has a major influence on the decision to breastfeed and on the duration of breastfeeding. Family and friends are often not aware of the importance of breastfeeding and how to be involved in the care and nurturing of a breastfed infant. Mothers should be encouraged to talk with their family and friends about breastfeeding and to invite them to attend prenatal classes to learn more about breastfeeding. Time and competing demands are a reality of life and new mothers can benefit from information on how breastfeeding can be successfully combined with other commitments in their busy lives. Statistics According to Tucker, Wilson, and Samandari (2011), in the United States, just over half of mothers under age 20 initiate breastfeeding. Furthermore, adolescents who
do initiate breastfeeding tend to breastfeed for shorter durations than older mothers. According to the National Immunization Survey, between 2004 and 2008 only 19% of teens continued to breastfeed at six months postpartum, compared with 34% of mothers ages 20-29 and 49% of women 30 and older. Several factors may explain the lower levels of breastfeeding among teen mothers. Given their age, teen mothers are more likely than older mothers to be single and to have lower levels of education and income--characteristics that are negatively associated with breastfeeding. Additional factors that may contribute to lower breastfeeding rates among teens include returning to school, unease with the act of breastfeeding, and embarrassment about breastfeeding in public. A lack of confidence in their ability to breastfeed and reticence to ask for help may be other barriers that pertain especially to teens. Current understanding of breastfeeding among adolescents has several limitations, however. Because national statistics group together mothers younger than 20, we do not have population-based data on the breastfeeding practices specific to younger school-age adolescents. In addition, most studies of adolescent breastfeeding are composed of hospital-based convenience samples of urban White and African American teens. As a result, available data focus primarily on breastfeeding intentions and decisions to initiate, and few studies examine breastfeeding experiences after hospital discharge. Furthermore, there is little information about breastfeeding experiences among Hispanic adolescents or among adolescents from rural areas in the United States.
According to Burks Aw (2010) that in the Philippines, the Implementing Rules and Regulations of the Milk Code requires that breastfeeding be encouraged for babies up to the age of 2 years old or beyond. Under the same code, it is prohibited to advertise infant formula or breast milk substitutes intended for infants and young children 24 months old and below. In practice, however, a 2008 WHO survey found that on average, mothers in the Philippines breastfed their babies until 14 months of age, with breastfeeding extending up to 17 months on average in rural areas. Almost fiftyeight percent of mothers surveyed around the nation were still breastfeeding their babies when the babies were a year old, and 34.2% of mothers were still breastfeeding when their babies were 2 years old. In 2012, it was reported that legislation had been introduced which would narrow down the application of the Milk Code (reducing the period recommending against artificial baby foods for babies from 0 to 36 months to 0 to six months only), would lift the restriction on donations of artificial milk products in emergency situations (encouraging mothers who suffer from disabilities to shift to milk substitutes instead of encouraging them to continue breastfeeding assisted by support persons), would change the legally mandated lactation break period for breastfeeding mothers from paid to unpaid status, and would remove the prohibition against milk companies giving away free samples of artificial milk products in the health care system. Confidence and self-efficacy According to Sjgren (2008), a woman who feels confident in her ability to breastfeed, to produce breast milk and who are motivated to breastfeed are more likely to have a longer duration of breastfeeding. When a woman worries about her ability to
breastfeed she can more easily loose her confidence and stop breastfeeding. The perceived ability influences the thoughts and actions of the individual and is therefore shown to be a predictor for her health behavior, writes Dennis (2000) in her article about self-efficacy. Dennis found that a high level of self-efficacy in breastfeeding leads to choosing, performing and maintaining breastfeeding as infant feeding method. Confidence and self-efficacy A woman who feels confident in her ability to breastfeed, to produce breast milk and who are motivated to breastfeed are more likely to have a longer duration of breastfeeding. When a woman worries about her ability to breastfeed she can more easily loose her confidence and stop breastfeeding (Sjgren, 2008). The perceived ability influences the thoughts and actions of the individual and is therefore shown to be a predictor for her health behavior, writes Dennis (2000) in her article about selfefficacy. Dennis found that a high level of self-efficacy in breastfeeding leads to choosing, performing and maintaining breastfeeding as infant feeding method. The Breastfeeding Self-efficacy Scale (BSES) has been developed by Dennis and Faux (1999) in Canada, with the objective to receive a predictor for breastfeeding initiation and duration. The results from assessing the scale showed that participants who rates their self-efficacy higher, more often exclusively breastfeed. A later study by Dennis (2003), also conducted in Canada, showed that the rates on the BSES have no correlation with demographic factors such as maternal age, education and income. In the BSES the woman answers questions about whether she chooses to breastfeed, how much effort she will provide in this task, how her thought pattern looks and how she will respond to difficulties. The answers to these questions show her confidence and
thereby can her breastfeeding duration be predicted (Dennis, 2000). According to Dennis and Faux the scale helps healthcare professional to identify mothers in risk of early discontinuing of breastfeeding and the healthcare professionals are thereby able to perform interventions. The predictive validity of the BSES has been further tested in a methodological study carried out in Australia by Creedy et al. (2003). This study supported the results of earlier studies that have indicated that BSES is a good predictor of infant feeding method. Creedy et al. (2003) suggested that a higher score on the BSES would be 140 and higher, and a lower score 130 and lower, but declared that more evaluation are needed. A study, conducted in Australia by Blyth et al. (2004) with the aim to investigate the influence of antenatal variables on breastfeeding outcome, used the BSES for exploring the confidence of the mothers in breastfeeding. The results indicated that most of the mothers felt confident in breastfeeding. Further the results revealed that the BSES score, also here, had a significant relation with breastfeeding duration and level. In Thailand, a study conducted by Bergstrm and Zyto (2009), also used the BSES for measuring mothers confidence in breastfeeding. The aim of the study was to investigate the attitude and confidence of breastfeeding mothers and showed that the Thai mothers had a good confidence in breastfeeding and a positive attitude to it. A study conducted in Sweden by Ekstrm, Widstrm and Nissen, (2007) had the objective to describe breastfeeding support and confidence in relation to breastfeeding duration. The results showed that one week after childbirth, first time mothers rated their confidence lower than mothers who had given birth before. The authors also showed a relation between the mothers confidence and her social support. An influence on
breastfeeding from grandmothers were shown, which brought Ekstrm et al. (2008) to the conclusion that healhcare professionals should include grandmothers who are positive to breastfeeding when supporting mothers. Vicarious experience Vicarious experience involves observing others performing activities and comparing oneself to them. This source of information can have a powerful impact on perceived self-efficacy especially in the absence of previous experience. Dennis (2002) concluded that the effect of observational learning is contingent on the attributes performed. Role modeling occurs when a woman watches breastfeeding or reads or hears about it. Friedman, (2008) gave an example that if the mother is watching great numbers of women successfully breastfeed their children in public places is role modeling and habituation that increases emotional comfort and more likely to choose and succeed at breastfeeding. According to Bandura (2009), this source of information usually provides weaker efficacy judgments than performance accomplishments, yet has the potential to provide important information. Verbal persuasion Through verbal persuasion, one is led through suggestion into increasing ones beliefs in ones capability. Bandura (2009), discussed that verbal persuasion must be realistic to contribute to ones beliefs about successful performance, and is only influential as the recipients confidence in the person issuing the information. Encouragements and evaluations from influential others such as lactation consultants, health professionals, peer counselors, and family members can be particularly beneficial to breastfeeding women. According to Dennis, (2000) a womans self-efficacy
is bolstered when attention is provided to the successful or improved aspects of breastfeeding performances. Physiological responses Bandura (2009) pointed out that physiological status involves ones interpretation of physical signs of arousal. Arousal is a result of the degree of perceived match between coping capabilities and task demands. So, how one perceives these signs of arousal determines the effect on performance and is affected by ones efficacy judgment. Emotional comfort is necessary for learning to take place. This area for breastfeeding mothers is of importance because increased anxiety has a direct effect on the milk ejection reflex and can decrease maternal milk supply. Breastfeeding Initiation Promotion of early initiation of breastfeeding has the potential to make a major contribution to the achievement of the child survival millennium development goal; 16% of neonatal deaths could be saved if all infants were breastfed from day 1 and 22% if breastfeeding started within the first hour. Breastfeeding-promotion programs should emphasize early initiation as well as exclusive breastfeeding. This has particular relevance for sub-Saharan Africa, where neonatal and infant mortality rates are high but most women already exclusively or predominantly breastfeed their infants. According to Alive & Thrive (2009), despite of the breastfeeding benefits, many women delay initiation of breastfeeding. Only 39 percent of newborns in developing countries are put to the breast within one hour of birth. Establishing good breastfeeding practices in the first days is critical to the health of the infant and to breastfeeding success. Initiating breastfeeding is easiest and most successful when a mother is
physically and psychologically prepared for birth and breastfeeding and when she is informed, supported, and confident of her ability to care for her newborn. The following actions can increase rates of early initiation of breastfeeding: Identify the practices, beliefs, concerns, and constraints to early and exclusive breastfeeding and address them through appropriate messages and changes in delivery and postpartum procedures; counsel women during antenatal care on early initiation and exclusive breastfeeding; upgrade the skills of trained attendants to support early and exclusive breastfeeding; make skin-to-skin contact and initiation of breastfeeding the first routine after delivery; practice the "Ten Steps to Successful Breastfeeding" in maternity services; praise the mother for giving colostrum, provide ongoing encouragement, and assist with positioning and attachment. Edmond et al (2006) concluded that breastfeeding was initiated within the first day of birth in 71% of infants and by the end of day 3 in all but 1.3% of them; 70% were exclusively breastfed during the neonatal period. The risk of neonatal death was fourfold higher in children given milk-based fluids or solids in addition to breast milk. There was a marked dose response of increasing risk of neonatal mortality with increasing delay in initiation of breastfeeding from 1 hour to day 7; overall late initiation (after day 1) was associated with a 2.4-fold increase in risk. The size of this effect was similar when the model was refitted excluding infants at high risk of death (unwell on the day of birth, congenital abnormalities, premature, unwell at the time of interview) or when deaths during the first week (days 27) were excluded. Exclusive Breastfeeding
According to World health Organization (2007), exclusive breastfeeding to six months of age has been one of the primary aims of nutrition and public health programs across the world. One of the Millennium Development Goal of WHO was to reduce child mortality by two-thirds, between 1990 and 2015, the under-five mortality rate. 6.9 million Children under five died in 2011. Almost 75% of all child deaths are attributable to just six conditions: neonatal causes, pneumonia, diarrhea, malaria, measles, and HIV/AIDS. The aim is to further cut child mortality by two thirds by 2015 from the 1990 level. UNICEF (2013) said that as a global goal for optimal maternal and child health and nutrition, all women should be enabled to practice exclusive breastfeeding and all infants should be fed exclusively on breast milk from birth to 4-6 months of age. Thereafter, children should continue to be breastfed, while receiving appropriate and adequate complementary foods, for up to two years of age or beyond. This child-feeding ideal is to be achieved by creating an appropriate environment of awareness and support so that women can breastfeed in this manner. CDC's Division of Nutrition, Physical Activity, and Obesity (DNPAO, 2009) is committed to increasing breastfeeding rates throughout the United States and to promoting and supporting optimal breastfeeding practices toward the ultimate goal of improving the public's health. Jun Pisco (2012) wrote in his article that the several international organizations hailed the Philippines for the significant increase in exclusive breastfeeding rates. Recent figures released by the Food and Nutrition Research Institute showed that exclusive breastfeeding rates have risen from 36 per cent in 2008 to 47 per cent in 2011. At the same time, there are still substantial disparities in exclusive breastfeeding rates within the Philippines. Data from the recent Family Health Survey (FHS) in 2011
showed that exclusive breastfeeding rates in some areas are as low as 27 per cent. Further efforts will be needed to increase the exclusive breastfeeding to be truly at the universal level, which will have a significant impact on the nutritional status of children in the Philippines. Exclusive breastfeeding is the best way to provide babies with the nutrients they need during the first six months of life, and means giving the baby no additional liquids or solid food - not even water. Predominant or mixed breastfeeding means feeding breast milk along with infant formula, baby food and even water, depending on the age of the child. Babies feed differently with artificial nipples than from a breast. With the breast, the infant's tongue massages the milk out rather than sucking, and the nipple does not go as far into the mouth; with an artificial nipple, an infant must suck harder and the milk may come in more rapidly. Therefore, mixing breastfeeding and bottle-feeding (or using a pacifier) before the baby is used to feeding from its mother can result in the infant preferring the bottle to the breast. Some mothers supplement feed with a small syringe or flexible cup to reduce the risk of artificial nipple preference. Planned breastfeeding and Decision to Breastfeed Although breastfeeding is beneficial to infant and mother, other factors are involved in the decision to breastfeed. In a study by Persad and Mensinger (2007), breastfeeding intent strongly correlated with breastfeeding initiation, indicating that women who decide to breastfeed during early pregnancy are likely to initiate lactation after birth. Brodribb, Fallon, Hegney, and OBrien (2007) reported that the women in their study decided whether or not to breastfeed before or in early pregnancy, and their decisions were based on baby- or mother-centered factors. The baby-centered factor
most frequently reported was concern for infant health. Mother-centered factors included either a preference to bottle-feed for convenience or a dislike of breastfeeding because of the reasons that included inconvenience, social barriers, or work-related barriers (Brodribb et al., 2007). Sociocultural, environmental, and personal factors are influential in a womans decision to breastfeed. If a woman perceives breastfeeding is the social norm, she may be more inclined to breastfeed. Throughout the literature, a recurring factor that influences a womans decision to breastfeed is the presence of a support system, whether it is personal or professional (Johnston & Esposito, 2007; Persad & Mensinger, 2007; Taveras, 2003). In fact, support systems may be a greater influence than socioeconomic status; if a woman views breastfeeding positively, and has support from her partner, she will be more likely to breastfeed (Persad & Mensinger, 2007). Additionally, the presence of professional support strongly correlates with both breastfeeding initiation (Persad & Mensinger, 2007) and increased duration of breastfeeding (Taveras et al., 2003). Professional support may include support from postpartum nurses during early hospitalization, lactation consultants, physicians (Johnston & Esposito, 2007), and clinicians, such as pediatricians and community lactation consultants outside the hospital (Taveras et al., 2003). Health-care workers during the immediate postpartum period, especially nurses and lactation consultants, play an integral role in assisting the mother to initiate breastfeeding. Education formally presented through individualized, interactional techniques rather than independent and informal means (such as pamphlets or other reading materials) usually yields better results (McInnes & Chambers, 2008; Persad & Mensinger, 2007; Swanson & Power, 2005). Clinicians who are in contact with the
mother and infant can affect the duration of breastfeeding by providing positive support, problem solving, and continued patient education. Because of the influence they have, it is important that clinicians have adequate knowledge and skills for educating and supporting women to increase the duration of breastfeeding (Taveras et al., 2003). A recurring factor that influences a womans decision to breastfeed is the presence of a support system, whether it is personal or professional. Race may also be a factor in initiation and duration of breastfeeding. Chin et al. (2008) found that, among the participants in their study, women of non-White racial backgrounds had lower initiation rates than White women. Additionally, the duration of breastfeeding among non-White women was shorter than among White women. Black women had both lower initiation and duration rates than White women regardless of other demographic and socioeconomic variables. Although several possible
explanations may explain this disparity, one reason is thought to be the early introduction of solid foods as a cultural norm (Chin et al., 2008). Conversely, Black women in the United Kingdom who recently immigrated from either the Caribbean or Africa were more likely to breastfeed at 3 months postpartum than White women (Kelly et al., 2006). The same was true of Indian and Bangladeshi mothers at 3 months, with the highest rate of breastfeeding in Black Caribbean women (Kelly et al., 2006). Women of higher educational status also have higher rates of breastfeeding. In the study by Chin et al. (2008), women who graduated from high school were 70% more likely to breastfeed than those who did not; women who attended college were four times more likely to breastfeed than women who graduated from high school. A
relationship between race and education could not be determined. In a national study of Canadian mothers, Chalmers et al. (2009) found women who were educated, older, had incomes above the low-income cutoff level, and had vaginal births were most likely to breastfeed. Marital status also affects breastfeeding initiation and duration. Compared to unmarried women, married women have higher rates of breastfeeding, especially among Black women. Married Black women are twice as likely to breastfeed as unmarried Black women (Chin et al., 2008; Thulier & Mercer, 2009). Synthesis Breastfeeding is a global issue for communities and governments that affect both women and their infants on many levels. Despite identifying factors that influence the initiation of breastfeeding and the importance of breastfeeding to both mother and infant, there continues to be sub-optimal exclusive breastfeeding in both developing and developed countries. National and international researchers, as well as governing bodies, have outlined guidelines that support and promote breastfeeding, strongly advocating breastfeeding as being the best practice by which to feed infants. Research shows the advantages to infants, mothers, families, and society from breastfeeding and the use of human milk for infant feeding. These include health, nutritional, immunologic, developmental, psychological, social, economic, and
environmental benefits. It has been observed that there is an important relationship between successful breastfeeding by the first-time mother and guidance and
encouragement on the part of health care professionals before and after the birth of the child. Although the health benefits of breastfeeding are well documented and initiation rates have increased over the past 20 years, most mothers wean before the recommended 6-months postpartum because of perceived difficulties with breastfeeding rather than due to maternal choice. Women least likely to breastfeed are those who are young, have a low income, belong to an ethnic minority, are unsupported, and are employed full-time, decided to breastfeed during or late in pregnancy, have negative attitudes toward breastfeeding, and have low confidence in their ability to breastfeed. Support from the mother's partner or a nonprofessional greatly increases the likelihood of positive breastfeeding behaviors. Health care professionals can be a negative source of support if their lack of knowledge results in inaccurate or inconsistent advice. Furthermore, a number of hospital routines are potentially detrimental to breastfeeding. Although professional interventions that enhance the usual care mothers receive increase breastfeeding duration to 2 months, these supportive strategies have limited long-term effects. Peer support interventions also promote positive breastfeeding behaviors and should be considered. The studies of American Association of Pediatric (AAP)(2007), Lawrence (2008), World Health Organization (2010), and Millenium Development Goals (2012) all stated that infants should be exclusively breastfeed for six months and according to them breastfeeding lowers the risk of different diseases like asthma, diarrhea, and respiratory illness. .
According to Ruth (2007), and Lawrence (2008) Therefore, researchers concluded that promotion and prolonging breastfeeding should positively modify the womans breastfeeding intention, her social support and her breastfeeding confidence.
También podría gustarte
- TRCN Paper 2Documento17 páginasTRCN Paper 2Chika JonesAún no hay calificaciones
- Breastfeeding Is Priceless: There Is No Substitute For Human MilkDocumento4 páginasBreastfeeding Is Priceless: There Is No Substitute For Human MilkmeetAún no hay calificaciones
- Notes On Exclusive BreastfeedingDocumento6 páginasNotes On Exclusive BreastfeedingNdem BasseyAún no hay calificaciones
- Benefits of Breast FeedingDocumento4 páginasBenefits of Breast FeedingAzAm KiOngAún no hay calificaciones
- Lits 1016 2Documento13 páginasLits 1016 2satraAún no hay calificaciones
- Assignment 2Documento7 páginasAssignment 2api-485256081Aún no hay calificaciones
- RESEARCH093016Documento28 páginasRESEARCH093016Satra Sabbuh100% (1)
- Breastfeeding Benefits HandoutDocumento4 páginasBreastfeeding Benefits Handoutapi-313912304Aún no hay calificaciones
- Benefits of Breastfeeding For Mothers - Nutr 251 Honors AssignmentDocumento10 páginasBenefits of Breastfeeding For Mothers - Nutr 251 Honors Assignmentapi-642953552Aún no hay calificaciones
- High Incidence of Exclusive Breastfeed Problems Among Working Mothers at Korle GonnoDocumento11 páginasHigh Incidence of Exclusive Breastfeed Problems Among Working Mothers at Korle GonnoMervin Boakye AgyemanAún no hay calificaciones
- Chapter1 4+breastfeeding+thesisDocumento31 páginasChapter1 4+breastfeeding+thesisJomel A. Garcia100% (1)
- Benefits of Exclusive Breastfeeding for BabiesDocumento6 páginasBenefits of Exclusive Breastfeeding for BabiesphobicmdAún no hay calificaciones
- Should WomenDocumento2 páginasShould Womenxena marie sumadiaAún no hay calificaciones
- Zainab ProjectDocumento35 páginasZainab ProjectOpeyemi JamalAún no hay calificaciones
- Community Nutrition Research PaperDocumento7 páginasCommunity Nutrition Research Paperapi-545176283Aún no hay calificaciones
- Thesis Statement Breastfeeding in PublicDocumento5 páginasThesis Statement Breastfeeding in Publicafkntwbla100% (2)
- Research Paper Topics On BreastfeedingDocumento5 páginasResearch Paper Topics On Breastfeedingafnhemzabfueaa100% (1)
- Ealth Cience Ournal: Cultural Views and Practices Related To BreastfeedingDocumento15 páginasEalth Cience Ournal: Cultural Views and Practices Related To BreastfeedingMiftahul JannahAún no hay calificaciones
- International Code of Marketing of BreastDocumento4 páginasInternational Code of Marketing of BreastSalsabil Sekar NabilaAún no hay calificaciones
- Exclusivebreastfeeding 181003124754Documento39 páginasExclusivebreastfeeding 181003124754apalanavedAún no hay calificaciones
- Thesis BreastfeedingDocumento5 páginasThesis BreastfeedingSteven Wallach100% (2)
- Annotated BibliographyDocumento5 páginasAnnotated Bibliographyapi-259924791Aún no hay calificaciones
- Breastfeeding A Womans Reproductive RightDocumento10 páginasBreastfeeding A Womans Reproductive RightMery Gomez LopezAún no hay calificaciones
- Breast FeedingDocumento43 páginasBreast FeedingFetria Melani50% (2)
- Does Homework Cause Childhood ObesityDocumento5 páginasDoes Homework Cause Childhood Obesityg3z6e4zm100% (1)
- Boado, Melody A. - NUPC108 - Assignment #1 (Finals)Documento3 páginasBoado, Melody A. - NUPC108 - Assignment #1 (Finals)Melody BoadoAún no hay calificaciones
- Chapter One 1.1 Background To The StudyDocumento44 páginasChapter One 1.1 Background To The StudyJustina Layo AgunloyeAún no hay calificaciones
- G NudDocumento17 páginasG NudBabangida AbubakarAún no hay calificaciones
- Breast Feeding Is The Normal Way of Providing Young Infants With The Nutrients They Need For Healthy Growth and DevelopmentDocumento8 páginasBreast Feeding Is The Normal Way of Providing Young Infants With The Nutrients They Need For Healthy Growth and Developmentdanee しAún no hay calificaciones
- My ThesisDocumento46 páginasMy ThesisManish SharmaAún no hay calificaciones
- Infant and Young Child Feeding: Key FactsDocumento5 páginasInfant and Young Child Feeding: Key FactsmalentotAún no hay calificaciones
- 12 Your Guide To BreastfeedingDocumento48 páginas12 Your Guide To Breastfeedingapi-309082881Aún no hay calificaciones
- Thesis On Exclusive BreastfeedingDocumento5 páginasThesis On Exclusive Breastfeedingebonybatesshreveport100% (2)
- Breastfeeding Education: Where Are We Going? A Systematic Review ArticleDocumento9 páginasBreastfeeding Education: Where Are We Going? A Systematic Review ArticleHaryaman JustisiaAún no hay calificaciones
- Drivers and Challenges of Exclusive Breastfeeding in West AfricaDocumento5 páginasDrivers and Challenges of Exclusive Breastfeeding in West AfricaKIU PUBLICATION AND EXTENSIONAún no hay calificaciones
- FAQ Code of Marketing of BMS 2008Documento18 páginasFAQ Code of Marketing of BMS 2008nikeAún no hay calificaciones
- Introduction Chapter I: 1.1 BackgroundDocumento9 páginasIntroduction Chapter I: 1.1 BackgroundOsob MohamudAún no hay calificaciones
- Materi MandiriDocumento6 páginasMateri Mandirip17311191006 RANINDYA DWI NOVIYANTIAún no hay calificaciones
- Chapter 1-3 ThesisDocumento20 páginasChapter 1-3 ThesisMarianne Gonzales100% (1)
- BF TSEK Slide Kit - 5july2012Documento31 páginasBF TSEK Slide Kit - 5july2012azuredreamAún no hay calificaciones
- Thesis RobinDocumento153 páginasThesis RobinPriyaAún no hay calificaciones
- Transcultural ChildbearingDocumento11 páginasTranscultural ChildbearingVerysa MaurentAún no hay calificaciones
- Knowledge Attitude and Practice of ExcluDocumento16 páginasKnowledge Attitude and Practice of ExclupblesynnAún no hay calificaciones
- Business Ethics NestleDocumento20 páginasBusiness Ethics NestleAnonymous Cm1mAb100% (2)
- BREASTFEEDINGDocumento28 páginasBREASTFEEDINGFiona Xandra San JuanAún no hay calificaciones
- Influence of Demographic Factors on Breastfeeding Practices in Anambra StateDocumento59 páginasInfluence of Demographic Factors on Breastfeeding Practices in Anambra StateIgbani Victory100% (1)
- Chapter 2 Review of Related LiteratureDocumento9 páginasChapter 2 Review of Related LiteratureKlei Vin DupianoAún no hay calificaciones
- 8 Maternal Nutrition During LactationDocumento28 páginas8 Maternal Nutrition During LactationEngga Swari RatihAún no hay calificaciones
- Breastfeeding Benefits Research PaperDocumento8 páginasBreastfeeding Benefits Research Paperafnhdcebalreda100% (1)
- NESTLE Case StudyDocumento7 páginasNESTLE Case StudyASAD ULLAHAún no hay calificaciones
- Factors Associated Early Termination of Exclusive Breastfeeding Among Infants Under Six MonthsDocumento9 páginasFactors Associated Early Termination of Exclusive Breastfeeding Among Infants Under Six MonthsAmedo Hajji MohamedAún no hay calificaciones
- Food Taboos and Misconceptions Among Pregnant Women of Shashemene District, Ethiopia, 2012Documento8 páginasFood Taboos and Misconceptions Among Pregnant Women of Shashemene District, Ethiopia, 2012Ramatu M BanguraAún no hay calificaciones
- Infant and Young Child FeedingDocumento5 páginasInfant and Young Child FeedingRinjaya TeguhAún no hay calificaciones
- Determinants of Breastfeeding Mother's in Obio/AkporDocumento16 páginasDeterminants of Breastfeeding Mother's in Obio/AkporNeat ScriptAún no hay calificaciones
- Cruz Final Grant ProposalDocumento40 páginasCruz Final Grant Proposalapi-341233003Aún no hay calificaciones
- BreastfeedingDocumento14 páginasBreastfeedingapi-302340748Aún no hay calificaciones
- A Critical Investigation On The Role of The Church in Supporting and Encouraging Nursing Mothers As Part of Its Holistic Mission in The Uk SummaryDocumento5 páginasA Critical Investigation On The Role of The Church in Supporting and Encouraging Nursing Mothers As Part of Its Holistic Mission in The Uk Summaryapi-249788544Aún no hay calificaciones
- Benefits of Breastfeeding for Infants and MothersDocumento3 páginasBenefits of Breastfeeding for Infants and MothersZ IAún no hay calificaciones
- Breastfeeding Benefits Baby's Health for LifeDocumento7 páginasBreastfeeding Benefits Baby's Health for LifevallikaAún no hay calificaciones
- Renderer InfosdfDocumento1 páginaRenderer Infosdfagulfam5542Aún no hay calificaciones
- Laboratory Values Case PressDocumento3 páginasLaboratory Values Case PressRoderick AgbuyaAún no hay calificaciones
- Fix Skyrim SKSE ErrorsDocumento4 páginasFix Skyrim SKSE ErrorsRoderick AgbuyaAún no hay calificaciones
- ARDS With PathophysiologyDocumento79 páginasARDS With Pathophysiologymabec pagaduan95% (19)
- VanityDocumento3 páginasVanityRoderick AgbuyaAún no hay calificaciones
- VanityDocumento3 páginasVanityRoderick AgbuyaAún no hay calificaciones
- Psych QuizDocumento3 páginasPsych QuizRoderick AgbuyaAún no hay calificaciones
- Pathophysiology ARDSDocumento1 páginaPathophysiology ARDSRoderick Agbuya100% (1)
- EAB Breastfeeding Final VersionDocumento73 páginasEAB Breastfeeding Final VersionRoderick AgbuyaAún no hay calificaciones
- Revised Disaster NursingDocumento25 páginasRevised Disaster NursingLlana Pauline JacintoAún no hay calificaciones
- Care of Patient With Acute Respiratory Distress SyndromeDocumento10 páginasCare of Patient With Acute Respiratory Distress SyndromeRoderick AgbuyaAún no hay calificaciones
- Case Format HahaDocumento5 páginasCase Format HahaRoderick AgbuyaAún no hay calificaciones
- There Are No ModBuddy Extensions YetDocumento1 páginaThere Are No ModBuddy Extensions YetRoderick AgbuyaAún no hay calificaciones
- Alloren Grace P (1) ThesisDocumento20 páginasAlloren Grace P (1) ThesisRoderick AgbuyaAún no hay calificaciones
- AssessmentDocumento1 páginaAssessmentRoderick AgbuyaAún no hay calificaciones
- Trigeminal NeurologiaDocumento45 páginasTrigeminal NeurologiaRoderick AgbuyaAún no hay calificaciones
- Chapter II Edited JeffDocumento20 páginasChapter II Edited JeffRoderick AgbuyaAún no hay calificaciones
- Bandura's Social Cognitive Theory and Self-EfficacyDocumento30 páginasBandura's Social Cognitive Theory and Self-EfficacyRoderick AgbuyaAún no hay calificaciones
- Respiratory Function TestDocumento7 páginasRespiratory Function TestMarivic DianoAún no hay calificaciones
- Nursing HistoryDocumento1 páginaNursing HistoryRoderick AgbuyaAún no hay calificaciones
- Bell's Palsy ReportDocumento25 páginasBell's Palsy ReportRoderick AgbuyaAún no hay calificaciones
- Mindanao's Epic Poetries Like Homer's Iliad and OdysseyDocumento1 páginaMindanao's Epic Poetries Like Homer's Iliad and OdysseyRoderick AgbuyaAún no hay calificaciones
- Esomeprazole (Nexium)Documento4 páginasEsomeprazole (Nexium)Roderick AgbuyaAún no hay calificaciones
- Count of Monte Cristo ReationDocumento2 páginasCount of Monte Cristo ReationRoderick AgbuyaAún no hay calificaciones
- Hiatal HerniaDocumento13 páginasHiatal HerniaRoderick AgbuyaAún no hay calificaciones
- Nursing Care Plan For Typhoid FeverDocumento1 páginaNursing Care Plan For Typhoid FeverRoderick Agbuya63% (8)
- Assessment of Respiratory FunctionDocumento1 páginaAssessment of Respiratory FunctionRoderick AgbuyaAún no hay calificaciones
- Mindanao's Epic Poetries Like Homer's Iliad and OdysseyDocumento1 páginaMindanao's Epic Poetries Like Homer's Iliad and OdysseyRoderick AgbuyaAún no hay calificaciones
- CSL AssignmentDocumento2 páginasCSL AssignmentMuhammad QubaisAún no hay calificaciones
- Repositioning Family Planning in Mali: A BaselineDocumento50 páginasRepositioning Family Planning in Mali: A BaselineFuturesGroup1Aún no hay calificaciones
- Causes of Obesity: Suzanne M. Wright, Louis J. AronneDocumento3 páginasCauses of Obesity: Suzanne M. Wright, Louis J. AronneCarla Fernanda Sanhueza PozoAún no hay calificaciones
- OGDocumento385 páginasOGMin MawAún no hay calificaciones
- 16CB01OIC0628Documento38 páginas16CB01OIC0628Satish GuptaAún no hay calificaciones
- Mission Indradhanush: Submitted By-Jayesh Agrawal Mba-Rural Development Semester-IstDocumento20 páginasMission Indradhanush: Submitted By-Jayesh Agrawal Mba-Rural Development Semester-IstJayeshAgrawalAún no hay calificaciones
- WHO Surgical Safety ChecklistDocumento1 páginaWHO Surgical Safety ChecklistArabelle GO100% (1)
- Name: Ala Sami Mahmoud Abusohyon Nationality: Jordanian: ObjectiveDocumento4 páginasName: Ala Sami Mahmoud Abusohyon Nationality: Jordanian: Objectiveamr ahmedAún no hay calificaciones
- A Snapshot of 2009: February 2010 Patient Groups' Views of PharmaDocumento12 páginasA Snapshot of 2009: February 2010 Patient Groups' Views of Pharmaapi-26153783Aún no hay calificaciones
- Caries TimelineDocumento11 páginasCaries TimelineManuelRomeroFAún no hay calificaciones
- Ordering Lab Tests: Alphabetical List of TestsDocumento3 páginasOrdering Lab Tests: Alphabetical List of TestsDjdjjd SiisusAún no hay calificaciones
- Case PresentationDocumento35 páginasCase Presentationapi-498720485Aún no hay calificaciones
- Alopecia Areata and Psoriasis Vulgaris Associated With TSDocumento3 páginasAlopecia Areata and Psoriasis Vulgaris Associated With TSILham SyahAún no hay calificaciones
- Kemampuan Clinical Reasoning Pada Ujian Osce Mahasiswa Kedokteran Tahun KetigaDocumento9 páginasKemampuan Clinical Reasoning Pada Ujian Osce Mahasiswa Kedokteran Tahun Ketigabelahan jiwaAún no hay calificaciones
- DR Moshiri - Class II Correction by Leveraging Molar Rotation - 2Documento4 páginasDR Moshiri - Class II Correction by Leveraging Molar Rotation - 2Enea NastriAún no hay calificaciones
- Clinical 1 Hand Washing Chimozi 1Documento6 páginasClinical 1 Hand Washing Chimozi 1Miriward ZimbaAún no hay calificaciones
- Drug Proving Project InvestigationsDocumento8 páginasDrug Proving Project InvestigationsJayAún no hay calificaciones
- Preterm Labor and PROMDocumento102 páginasPreterm Labor and PROMDan Matthew BuriasAún no hay calificaciones
- Ethics Gtu 301 Final Exam.14.15 1Documento2 páginasEthics Gtu 301 Final Exam.14.15 1JebatAl-KelantaniAún no hay calificaciones
- COVID-19 Vaccine Mechanisms and ImmunityDocumento1 páginaCOVID-19 Vaccine Mechanisms and ImmunityAvinash KumbharAún no hay calificaciones
- VIII - PMHN Role As A Member of The Research TeamDocumento15 páginasVIII - PMHN Role As A Member of The Research Teamlester lopezAún no hay calificaciones
- Journal - Bacteria Virtual LabDocumento1 páginaJournal - Bacteria Virtual Labapi-348935712Aún no hay calificaciones
- Aug-Sept'12 IHP HoxseyFormula MonographDocumento1 páginaAug-Sept'12 IHP HoxseyFormula Monographterryvnd100% (1)
- Handouts - Dr. Ahmed Leithey - Management of Endodontically Treated TeethDocumento8 páginasHandouts - Dr. Ahmed Leithey - Management of Endodontically Treated TeethAbdelfattah EL KadyAún no hay calificaciones
- Moot Proposition On Health Law 1Documento3 páginasMoot Proposition On Health Law 1Pranav BhaskarAún no hay calificaciones
- Job Description of Nursing OfficerDocumento12 páginasJob Description of Nursing OfficerPunam DuwalAún no hay calificaciones
- Cbahi Esr StandardDocumento7 páginasCbahi Esr StandardSitti Frizaida AininAún no hay calificaciones
- NCP DRDocumento3 páginasNCP DRRhuwelyn Parantar PilapilAún no hay calificaciones
- Running Head: Evidence-Based Practice: Pressure Ulcer RiskDocumento5 páginasRunning Head: Evidence-Based Practice: Pressure Ulcer RiskElise HowardAún no hay calificaciones
- Leprosy (Morbus Hansen) : Dr. Uun Khusnul Khotimah, SPKKDocumento38 páginasLeprosy (Morbus Hansen) : Dr. Uun Khusnul Khotimah, SPKKagilAún no hay calificaciones