Documentos de Académico
Documentos de Profesional
Documentos de Cultura
A
Cargado por
rezadutTítulo original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
A
Cargado por
rezadutCopyright:
Formatos disponibles
Background Acute diarrhea is defined as the abrupt onset of 3 or more loose stools per day.
The augmented water content in the stools (above the normal value of approximately 10 mL/kg/d in the infant and young child, or 200 g/d in the teenager and adult) is due to an imbalance in the physiology of the small and large intestinal processes involved in the absorption of ions, organic substrates, and thus water. A common disorder in its acute form, diarrhea has many causes and may be mild to severe. Childhood acute diarrhea is usually caused by infection of the small and/or large intestine; however, numerous disorders may result in diarrhea, including a malabsorption syndrome and various enteropathies. Acute-onset diarrhea is usually self-limited; however, an acute infection can have a protracted course. By far, the most common complication of acute diarrhea is dehydration. Although the term "acute gastroenteritis" is commonly used synonymously with "acute diarrhea," the former term is a misnomer. The term gastroenteritis implies inflammation of both the stomach and the small intestine, whereas, in reality, gastric involvement is rarely if ever seen in acute diarrhea (including diarrhea with an infectious origin); in addition, enteritis is also not consistently present. Examples of infectious acute diarrhea syndromes that do not cause enteritis include Vibrio cholerae induced diarrhea and Shigella -induced diarrhea. Thus, the term acute diarrhea is preferable to acute gastroenteritis. Diarrheal episodes are classically distinguished into acute and chronic (or persistent) based on their duration. Acute diarrhea is thus defined as an episode that has an acute onset and lasts no longer than 14 days; chronic or persistent diarrhea is defined as an episode that lasts longer than 14 days. The distinction, supported by the World Health Organization (WHO), has implications not only for classification and epidemiological studies but also from a practical standpoint because protracted diarrhea often has a different set of causes, poses different problems of management, and has a different prognosis. Pathophysiology Diarrhea is the reversal of the normal net absorptive status of water and electrolyte absorption to secretion. Such a derangement can be the result of either an osmotic force that acts in the lumen to drive water into the gut or the result of an active secretory state induced in the enterocytes. In the former case, diarrhea is osmolar in nature, as is observed after the ingestion of nonabsorbable sugars such as lactulose or lactose in lactose malabsorbers. Instead, in the typical active secretory state, enhanced anion secretion (mostly by the crypt cell compartment) is best exemplified by enterotoxin-induced diarrhea. In osmotic diarrhea, stool output is proportional to the intake of the unabsorbable substrate and is usually not massive; diarrheal stools promptly regress with discontinuation of the offending nutrient, and the stool ion gap is high, exceeding 100 mOsm/kg. In fact, the fecal osmolality in this circumstance is accounted for not only by the electrolytes but also by the unabsorbed nutrient(s) and their degradation products. The ion gap is obtained by subtracting the concentration of the electrolytes from total osmolality (assumed to be 290 mOsm/kg), according to the formula: ion gap = 290 [(Na + K) 2]. In secretory diarrhea, the epithelial cells ion transport processes are turned into a state of active secretion. The most common cause of acute-onset secretory diarrhea is a bacterial infection of the gut. Several mechanisms may be at work. After colonization, enteric pathogens may adhere to or invade the epithelium; they may produce enterotoxins (exotoxins that elicit secretion by increasing an intracellular second messenger) or cytotoxins. They may also trigger release of cytokines attracting inflammatory cells, which, in turn, contribute to the activated secretion by inducing the release of agents such as prostaglandins or platelet-activating factor. Features of secretory diarrhea include a high purging rate, a lack of response to fasting, and a normal stool ion gap (ie, 100 mOsm/kg or less), indicating that nutrient absorption is intact. Epidemiology Frequency United States In the United States, one estimate before the introduction of specific antirotavirus immunization in 2006 assumed a cumulative incidence of 1 hospitalization for diarrhea per 23-27 children by age 5 years, with more than 50,000 hospitalizations. By these estimates, rotavirus was associated with 4-5% of all
childhood hospitalizations and a cost of nearly $ 1 billion.[1] Furthermore, acute diarrhea is responsible for 20% of physician referrals in children younger than 2 years and for 10% in children younger than 3 years. The impact of vaccination on rotavirus morbidity has been remarkable, with significant reduction of diarrhea-associated hospitalizations and visits to emergency departments in children in the years 20072008 compared with the prevaccine period.[2] International In developing countries, an average of 3 episodes per child per year in children younger than 5 years is reported; however, some areas report 6-8 episodes per year per child. In these settings, malnutrition is an important additional risk factor for diarrhea, and recurrent episodes of diarrhea lead to growth faltering and substantially increased mortality.[3] Childhood mortality associated with diarrhea has constantly but slowly declined during the past 2 decades, mostly because of the widespread use of oral rehydration solutions; however, it appears to have plateaued over the past several years. Because the single most common cause of infectious diarrhea worldwide is rotavirus, and because a vaccine has been in use for over 3 years now, a reduction in the overall frequency of diarrheal episodes is hoped for in the near future. Mortality/Morbidity Mortality from acute diarrhea is overall globally declining but remains high. Most estimates have diarrhea as the second cause of childhood mortality, with 18% of the 10.6 million yearly deaths in children younger than age 5 years. Despite a progressive reduction in global diarrheal disease mortality over the past 2 decades, diarrhea morbidity in published reports from 1990-2000 slightly increased worldwide compared with previous reports. In the United States, an average of 369 diarrhea-associated deaths/year occurred among children aged 1-59 months during 1992-1998 and 2005-2006.[4] The vast majority of diarrhea-associated infant deaths were reported in 2005-2007, with 86% of deaths occurring among low-birthweight (< 2500 g) infants.[5] Furthermore, in countries in which the toll of diarrhea is highest, poverty also adds an enormous additional burden, and long-term consequences of the vicious cycle of enteric infections, diarrhea, and malnutrition are devastating.[3] Sex Most cases of infectious diarrhea are not sex specific. Females have a higher incidence of Campylobacter species infections and hemolytic uremic syndrome (HUS). Age Viral diarrhea is most common in young children. Rotavirus and adenovirus are particularly prevalent in children younger than 2 years. Astrovirus and norovirus usually infect children younger than 5 years. Yersinia enterocolitis typically infects children younger than 1 year, and the Aeromonas organism is a significant cause of diarrhea in young children. Very young children are particularly susceptible to secondary dehydration and secondary nutrient malabsorption. Age and nutritional status appear to be the most important host factors in determining the severity and the duration of diarrhea. In fact, the younger the child, the higher is the risk for severe, lifethreatening dehydration as a result of the high body-water turnover and limited renal compensatory capacity of very young children. Whether younger age also means a risk of running a prolonged course is an unsettled issue. In developing countries, persistent postenteritis diarrhea has a strong inverse correlation with age. History Acute diarrhea in developed countries is almost invariably a benign, self-limited condition, subsiding within a few days. The clinical presentation and course of illness depend on the etiology of the diarrhea and on the host. For example, rotavirus is more commonly associated with vomiting, dehydration, and a greater number of work days lost than nonrotavirus gastroenteritis. A prospective study conducted in the United States in 604 children aged 3-36 months in community settings before the introduction of rotavirus vaccine found that the highest incidence of acute diarrhea was in January and August, with an overall incidence of 2.21 episodes per
person-year.[6] Close to 90% of episodes were acute (ie, lasting < 14 d, with a median duration of 2 d and a median of 6 stools per day). Diarrhea implies an increase in stool volume and diminished stool consistency. o In children younger than 2 years, diarrhea is defined as daily stools with a volume greater than 10 mL/kg. o In children older than 2 years, diarrhea is defined as daily stools with a weight greater than 200 g. In practice, this typically means loose-to-watery stools passed 3 or more times per day. o Individual stool patterns widely vary; for example, breastfed children may normally have 5-6 stools per day. Flatulence associated with foul-smelling stools that float suggests fat malabsorption, which can be observed with infection with Giardia lamblia. Knowledge of the characteristics of consistency, color, volume, and frequency can be helpful in determining whether the source is from the small or large bowel. Table 1 outlines these characteristics and demonstrates that an index of suspicion can be easily generated for a specific set of organisms. Table 1. Stool Characteristics and Determining Their Source (Open Table in a new window) Stool Small Bowel Large Bowel Characteristics Watery Mucoid and/or bloody Appearance Large Small Volume Increased Highly increased Frequency Possibly positive but never gross Commonly grossly bloody Blood blood Possibly < 5.5 >5.5 pH Possibly positive Negative Reducing substances < 5/high power field Commonly >10/high power field WBCs Normal Possible leukocytosis, bandemia Serum WBCs Organisms Viral Invasive bacteria Rotavirus Escherichia Coli (enteroinvasive, Adenovirus enterohemorrhagic) Calicivirus Shigella species Astrovirus Salmonella species Norovirus Campylobacter species Yersinia species Aeromonas species Plesiomonas species Enterotoxigenic bacteria Toxic bacteria E coli Clostridium difficile Klebsiella Clostridium perfringens Cholera species Vibrio species Parasites Parasites Giardia species Entamoeba organisms Cryptosporidium species
Associated systemic symptoms include the following: o Some enteric infections commonly have systemic symptoms, whereas others less commonly are associated with systemic features. o Table 2 outlines the frequency of some of these symptoms with particular organisms. It also outlines incubation periods and usual duration of symptoms of common organisms. Certain organisms (eg, C difficile, Giardia, Entamoeba species) may be associated with a protracted course. Table 2. Organisms and Frequency of Symptoms (Open Table in a new window) Organism Incubation Duration Vomiting Fever Abdominal Pain 1-7 d 4-8 d Yes Low No Rotavirus 8-10 d 5-12 d Delayed Low No Adenovirus 1-2 d 2d Yes No No Norovirus 1-2 d 4-8 d +/+/No Astrovirus 1-4 d 4-8 d Yes +/No Calicivirus None 0-2 wk +/+/No Aeromonas species 2-4 d 5-7 d No Yes Yes Campylobacter species Variable Variable No Few Few C difficile Minimal 1d Mild No Yes C perfringens 3-6 d No +/Yes Enterohemorrhagic E coli 1-8 d 1-3 d 3-5 d Yes Low Yes Enterotoxigenic E coli None 0-2 wk +/+/+/Plesiomonas species 0-3 d 2-7 d Yes Yes Yes Salmonella species 0-2 d 2-5 d No High Yes Shigella species 0-1 d 5-7 d Yes No Yes Vibrio species None 1-46 d Yes Yes Yes Y enterocolitica 2 wk 1+ wk No No Yes Giardia species Months No Low Yes Cryptosporidium species 5-21 d 5-7 d 1-2+ wk No Yes No Entamoeba species Daycare considerations are as follows: o Certain organisms are spread quickly in daycare. These organisms include rotavirus; astrovirus; calicivirus; and Campylobacter, Shigella, Giardia, and Cryptosporidium species. o Increase in daycare usage has raised the incidence of rotavirus and Cryptosporidium species. Food history can be helpful. o Ingestion of raw or contaminated food is a common cause of infectious diarrhea. o Organisms that cause food poisoning include the following: Dairy food -Campylobacter and Salmonella species Eggs -Salmonella species Meats -C perfringens and Aeromonas, Campylobacter, and Salmonella species Ground beef - Enterohemorrhagic E coli Poultry -Campylobacter species Pork -C perfringens, Y enterocolitica Seafood - Astrovirus and Aeromonas, Plesiomonas, and Vibrio species Oysters - Calicivirus and Plesiomonas and Vibrio species Vegetables -Aeromonas species and C perfringens
Water exposure can contribute to diarrhea. o Water is a major reservoir for many organisms that cause diarrhea. o Swimming pools have been associated with outbreaks of infection with Shigella species; Aeromonas organisms are associated with exposure to the marine environment. o Giardia, Cryptosporidium, and Entamoeba organisms are resistant to water chlorination; therefore, exposure to contaminated water should raise index of suspicion for these parasites. A history of camping suggests exposure to water sources contaminated with Giardia organisms. Travel history may indicate a cause for diarrhea. o Enterotoxigenic E coli is the leading cause of traveler's diarrhea. o Rotavirus and Shigella, Salmonella, and Campylobacter organisms are prevalent worldwide and need to be considered regardless of specific travel history. o Risk of contracting diarrhea while traveling is, by far, highest for persons traveling to Africa. o Travel to Central and South America and Eastern European countries is also associated with a relatively high risk of contracting diarrhea. o Other organisms that are prevalent in particular parts of the world include the following: Nonspecific foreign travel history - Enterotoxigenic E coli and Aeromonas, Giardia, Plesiomonas, Salmonella, and Shigella species Underdeveloped tropical visit -C perfringens Travel to Africa -Entamoeba species, Vibrio cholerae Travel to South America and Central America -Entamoeba species, V cholerae, enterotoxigenic E coli Travel to Asia -V cholerae Travel to Australia -Yersinia species Travel to Canada -Yersinia species Travel to Europe -Yersinia species Travel to India -Entamoeba species, V cholerae Travel to Japan -Vibrio parahaemolyticus Travel to Mexico -Aeromonas, Entamoeba, Plesiomonas, and Yersinia species New Guinea -Clostridium species Animal exposure can contribute to diarrhea. o Exposure to young dogs or cats is associated with Campylobacter organisms. o Exposure to turtles is associated with Salmonella organisms. Certain medical conditions predispose patients to infection, including the following: o C difficile - Hospitalization, antibiotic administration o Plesiomonas species - Liver diseases or malignancy o Salmonella species - Intestinal dysmotility, malnutrition, achlorhydria, hemolytic anemia (especially sickle cell disease), immunosuppression, malaria o Rotavirus - Hospitalization o Giardia species -Agammaglobulinemia, chronic pancreatitis, achlorhydria, cystic fibrosis o Cryptosporidia species - Immunocompromised or immunosuppressed state Physical The following may be observed: Dehydration o Dehydration is the principal cause of morbidity and mortality. o Assess every patient with diarrhea for signs, symptoms, and severity. o Lethargy, depressed consciousness, sunken anterior fontanel, dry mucous membranes, sunken eyes, lack of tears, poor skin turgor, and delayed capillary refill are obvious and important signs of dehydration. Table 3 below details dehydration severity and symptoms.
Table 3. Dehydration Severity, Signs, and Symptoms (Open Table in a new window) Hydration 0-5% Dehydration 5-10% Dehydration 10% or More
(Mild)
(Moderate)
(Severe)
Restless Lethargic General Well Normal Sunken Very sunken Eyes Present Absent Absent Tears Moist Dry Very dry Mouth Drinks normally Thirsty Drinks poorly Thirst Pinch retracts immediately Pinch retracts slowly Pinch stays folded Skin Failure to thrive and malnutrition o Reduced muscle and fat mass or peripheral edema may be clues to the presence of carbohydrate, fat, and/or protein malabsorption. o Giardia organisms can cause intermittent diarrhea and fat malabsorption. Abdominal pain o Nonspecific nonfocal abdominal pain and cramping are common with some organisms. o Pain usually does not increase with palpation. o With focal abdominal pain worsened by palpation, rebound tenderness, or guarding, be alert for possible complications or for another noninfectious diagnosis. Borborygmi: Significant increases in peristaltic activity can cause an audible and/or palpable increase in bowel activity. Perianal erythema o Frequent stools can cause perianal skin breakdown, particularly in young children. o Secondary carbohydrate malabsorption often results in acidic stools. o Secondary bile acid malabsorption can result in a severe diaper dermatitis that is often characterized as a "burn." Causes Although infectious agents are by far the most common cause for sporadic or endemic episodes of acute diarrhea, one should not dismiss other causes that can lead to the same presentation. Causes of diarrhea with acute onset include the following: o Infections Enteric infections (including food poisoning Extraintestinal infections o Drug-induced Antibiotic-associated Laxatives Antacids that contain magnesium Opiate withdrawal Other drugs o Food allergies or intolerances Cow's milk protein allergy Soy protein allergy Multiple food allergies Olestra Methylxanthines (caffeine, theobromine, theophylline)
Disorders of digestive/absorptive processes Glucose-galactose malabsorption Sucrase-isomaltase deficiency Late-onset (adult-type) hypolactasia, resulting in lactose intolerance o Chemotherapy or radiation-induced enteritis o Surgical conditions Acute appendicitis Intussusception o Vitamin deficiencies Niacin deficiency Folate deficiency o Vitamin toxicity Vitamin C Niacin, vitamin B3 o Ingestion of heavy metals or toxins (eg, copper, tin, zinc) o Ingestion of plants (eg, hyacinths, daffodils, azalea, mistletoe, Amanita species mushrooms Infectious causes of acute diarrhea in developed countries o Viruses Rotavirus - 25-40% of cases Norovirus - 10-20% of cases Calicivirus - 1-20% of cases Astrovirus - 4-9% of cases Enteric-type adenovirus - 2-4% of cases o Bacteria Campylobacter jejuni - 6-8% of cases Salmonella - 3-7% of cases E Coli - 3-5% of cases Shigella - 0-3% of cases Y enterocolitica - 1-2% of cases C difficile - 0-2% of cases Vibrio parahaemolyticus - 0-1% of cases V cholerae - Unknown Aeromonas hydrophila - 0-2% of cases o Parasites Cryptosporidium - 1-3% of cases G lamblia - 1-3% of cases Differential Diagnoses Appendicitis Carcinoid Tumor Congenital Microvillus Atrophy Crohn Disease Cystic Fibrosis Giardiasis Glucose-galactose malabsorption Hyperthyroidism Intestinal Enterokinase Deficiency Intestinal Protozoal Diseases Intussusception Irritable Bowel Syndrome Malabsorption Syndromes
Meckel Diverticulum Protein Intolerance Shigella Infection Short Bowel Syndrome Ulcerative Colitis Laboratory Studies The following may be noted in patients with diarrhea: In patients with diarrhea, a stool pH level of 5.5 or less or presence of reducing substances indicates carbohydrate intolerance, which is usually secondary to viral illness and transient in nature. Enteroinvasive infections of the large bowel cause leukocytes, predominantly neutrophils, to be shed into stool. Absence of fecal leukocytes does not eliminate the possibility of enteroinvasive organisms. However, presence of fecal leukocytes eliminates consideration of enterotoxigenic E coli, Vibrio species, and viruses. Examine any exudates found in stool for leukocytes. Such exudates highly suggest colitis (80% positive predictive value). Colitis can be infectious, allergic, or part of inflammatory bowel disease (Crohn disease, ulcerative colitis). Many different culture mediums are used to isolate bacteria. Table 3 lists common bacteria and optimum culture mediums for their growth. A high index of suspicion is needed to choose the appropriate medium. With stool not cultured within 2 hours of collection, refrigerate at 4C or place in a transport medium. Although stool cultures are useful when positive, yield is low. Always culture stool for Salmonella, Shigella, and Campylobacter organisms and Y enterocolitica in the presence of clinical signs of colitis or if fecal leucocytes are found. Look for C difficile in persons with episodes of diarrhea characterized by colitis and/or blood in the stools. Remember that acute-onset diarrheal episodes associated with C difficile may also occur without a history of antibiotic use. Bloody diarrhea with a history of ground beef ingestion must raise suspicion for enterohemorrhagic E coli. If E coli is found in the stool, determine if the type of E coli is O157:H7. This type of E coli is the most common, but not only, cause of HUS. History of raw seafood ingestion or foreign travel should prompt additional screening for Vibrio and Plesiomonas species. Table 4. Common Bacteria and Optimum Culture Mediums (Open Table in a new window) Organism Detection Method Microbiologic Characteristics Aeromonas Blood agar Oxidase-positive flagellated gram-negative species bacillus (GNB) Campylobacter Skirrow agar Rapidly motile curved gram-negative rod species (GNR); Campylobacter jejuni 90% and Campylobacter coli 5% of infections C difficile Cycloserine-cefoxitin-fructose-egg Anaerobic spore-forming gram-positive rod (CCFE) agar; enzyme immunoassay (GPR); toxin-mediated diarrhea; produces (EIA) for toxin; latex agglutination (LA) pseudomembranous colitis for protein C perfringens None available Anaerobic spore-forming GPR; toxinmediated diarrhea E coli MacConkey eosin-methylene blue (EMB) Lactose-producing GNR or Sorbitol-MacConkey (SM) agar Plesiomonas Blood agar Oxidase-positive GNR species
Salmonella species
Blood, MacConkey EMB, xylose-lysine- Nonlactose nonH2S-producing GNR deoxycholate (XLD), or Hektoen enteric (HE) agar Culture mediums used to isolate bacteria include the following: o Blood agar - All aerobic bacteria and yeast; detects cytochrome oxidase production o MacConkey EMB agar - Inhibits gram-positive organisms; permits lactose fermentation o XLD agar; HE agar - Inhibits gram-positive organisms and nonpathogenic GNB; permits lactose fermentation H2S production o Skirrow agar - Selective for Campylobacter species o SM agar - Selective for enterohemorrhagic E coli o CIN agar - Selective for Y enterocolitica o TCBS agar - Selective for Vibrio species o CCFE agar - Selective for C difficile Rotavirus antigen can be identified by enzyme immunoassay and latex agglutination assay of the stool. The false-negative rate is approximately 50%, and false-positive results occur, particularly in the presence of blood in the stools. Adenovirus antigens can be detected by enzyme immunoassay. Only serotypes 40 and 41 are able to induce diarrhea. Examination of stools for ova and parasites is best for finding parasites. Perform stool examination every 3 days or every other day. The leukocyte count is usually not elevated in viral-mediated and toxin-mediated diarrhea. Leukocytosis is often but not constantly observed with enteroinvasive bacteria. Shigella organisms cause a marked bandemia with a variable total white blood cell count. At times, a protein-losing enteropathy can be found in patients with extensive inflammation in the course of enteroinvasive intestinal infections (eg, Salmonella species, enteroinvasive E coli). In these circumstances, low serum albumin levels and high fecal alpha1-antitrypsin levels can be found. Other Tests Because the pathogenesis of diarrhea can be either osmolar (due to the presence of an excess of unabsorbed substrates in the gut lumen) or secretory (due to active anion secretion from the enterocytes), the anion gap in the stools is occasionally used to ascertain the nature of the diarrhea. The stool anion gap is calculated according to the formula: 290 - [(Na+K) X 2]. If the value is more than 100, osmolar diarrhea can be assumed to be present. If the value is less than 100, the diarrhea has a secretory origin. Procedures Intestinal biopsy is not required in evaluating an otherwise healthy child with acute-onset diarrhea, but it may be indicated in the presence of chronic or protracted diarrhea, as well as in cases in which a search for a cause is believed to be mandatory (eg, in patients with acquired immunodeficiency syndrome [AIDS] or patients who are otherwise severely immunocompromised). Medical Care In 2003 the Center for Disease Control (CDC) put forth recommendations for the management of acute pediatric diarrhea in both the outpatient and inpatient settings including indication for referral. [7] Indications for medical evaluation of children with acute diarrhea include the following: Younger than 3 months Weight of less than 8 kg History of premature birth, chronic medical conditions, or concurrent illness Fever of 38C or higher in infants younger than 3 months or 39C or higher in children aged 3-36 months Visible blood in the stool High-output diarrhea Persistent emesis
Signs of dehydration as reported by caregiver, including sunken eyes, decreased tears, dry mucous membranes, and decreased urine output Mental status changes Inadequate responses to oral rehydration therapy (ORT) or caregiver unable to administer ORT The report also includes information on assessment of dehydration and what steps should be taken to adequately treat acute diarrhea. Treatment of dehydration due to diarrhea includes the following: Minimal or no dehydration o Rehydration therapy - Not applicable o Replacement of losses Less than 10 kg body weight - 60-120 mL oral rehydration solution for each diarrhea stool or vomiting episode More than 10 kg body weight - 120-140 mL oral rehydration solution for each diarrhea stool or vomiting episode Mild-to-moderate dehydration o Rehydration therapy - Oral rehydration solution (50-100 mL/kg over 3-4 h) o Replacement of losses Less than 10 kg body weight - 60-120 mL oral rehydration solution for each diarrhea stool or vomiting episode More than 10 kg body weight - 120-140 mL oral rehydration solution for each diarrhea stool or vomiting episode Severe dehydration o Rehydration therapy - Intravenous lactated Ringer solution or normal saline (20 mL/kg until perfusion and mental status improve), followed by 100 mL/kg oral rehydration solution over 4 hours or 5% dextrose (half normal saline) intravenously at twice maintenance fluid rates o Replacement of losses Less than 10 kg body weight - 60-120 mL oral rehydration solution for each diarrhea stool or vomiting episode More than 10 kg body weight - 120-140 mL oral rehydration solution for each diarrhea stool or vomiting episode If unable to drink, administer through nasogastric tube or intravenously administer 5% dextrose (one fourth normal saline) with 20 mEq/L potassium chloride ORT is the cornerstone of treatment, especially for small-bowel infections that produce a large volume of watery stool output. ORT with a glucose-based oral rehydration syndrome must be viewed as by far the safest, most physiologic, and most effective way to provide rehydration and maintain hydration in children with acute diarrhea worldwide, as recommended by the WHO; by the ad hoc committee of European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN); and by the American Academy of Pediatrics.[8] However, the global use of ORT is still insufficient. Developed countries, in particular the United States, seem to be lagging behind despite studies that demonstrate beyond doubt the efficacy of ORT in emergency care settings, in which intravenous rehydration unduly continues to be widely privileged. Not all commercial ORT formulas promote optimal absorption of electrolytes, water, and nutrients. The ideal solution has a low osmolarity (210-250) and a sodium content of 50-60 mmol/L. Administer maintenance fluids plus replacement of losses. Educate caregivers in methods necessary to replace this amount of fluid. Administer small amounts of fluid at frequent intervals to minimize discomfort and vomiting. A 5-mL or 10-mL syringe without a needle is a very useful tool. The syringe can be quickly used to place small amounts of fluid in the mouth of a child who is uncooperative. Once the child becomes better hydrated, cooperation improves enough to take small sips from a cup. This method is time
intensive and requires a dedicated caregiver. Encouragement from the physician is necessary to promote compliance. Oral rehydration is now universally recommended to be completed within 4 hours. The addition of zinc to oral rehydration solution has been proven effective in children with acute diarrhea in developing countries and is recommended by the WHO.[9] However, no evidence suggests efficacy in children living in developed countries, in which the prevalence of zinc deficiency is assumed to be extremely low. The composition of almost all other beverages (carbonated or not) that are commercially available and frequently used in children with diarrhea is completely inadequate for rehydration or for maintaining hydration, considering the sodium content, which is invariably extremely low, and osmolarity that is often dangerously elevated. For instance, Coca-Cola, Pepsi-Cola, and apple juice have an osmolarity of 493, 576, and 694-773, respectively. At completion of hydration, resumption of feeding is strongly recommended. In fact, many studies convincingly demonstrate that early refeeding hastens recovery. Also, robust evidence suggests that, in the vast majority of episodes of acute diarrhea, refeeding can be accomplished without the use of any special (eg, lactose-free or soy-based) formulas. Antimotility agents are not indicated for infectious diarrhea, except for refractory cases of Cryptosporidium infection. Antimicrobial therapy is indicated for some nonviral diarrhea because most is self-limiting and does not require therapy. Therapies recommended for some nonviral diarrheas include the following: Aeromonas species: Use cefixime and most third-generation and fourth-generation cephalosporins. Campylobacter species: Erythromycin shortens illness duration and shedding. C difficile: Discontinue potential causative antibiotics. If antibiotics cannot be stopped or this does not result in resolution, use oral metronidazole or vancomycin. Vancomycin is reserved for the child who is seriously ill. C perfringens: Do not treat with antibiotics. Cryptosporidium parvum: Administer paromomycin; however, effectiveness is not proven. Nitazoxanide, a newer anthelmintic, is effective against C parvum. Entamoeba histolytica: Metronidazole followed by iodoquinol or paromomycin is administered in symptomatic patients. Asymptomatic carriers in nonendemic areas should receive iodoquinol or paromomycin. E coli: Trimethoprim-sulfamethoxazole (TMP-SMX) should be administered if moderate or severe diarrhea is noted; antibiotic treatment may increase likelihood of hemolytic-uremic syndrome (HUS). Parenteral second-generation or third-generation cephalosporin is indicated for systemic complications. G lamblia: Metronidazole or nitazoxanide can be used. Plesiomonas species: Use TMP-SMX or any cephalosporin. Salmonella species: Treatment prolongs carrier state, is associated with relapse, and is not indicated for nontyphoid-uncomplicated diarrhea. Treat infants younger than 3 months and highrisk patients (eg, immunocompromised, sickle cell disease). TMP-SMX is first-line medication; however, resistance occurs. Use ceftriaxone and cefotaxime for invasive disease. Shigella species: Treatment shortens illness duration and shedding but does not prevent complications. TMP-SMX is first-line medication; however, resistance occurs. Cefixime, ceftriaxone, and cefotaxime are recommended for invasive disease. V cholerae: Treat infected individuals and contacts. Doxycycline is the first-line antibiotic, and erythromycin is second-line antibiotic. Yersinia species: TMP-SMX, cefixime, ceftriaxone, and cefotaxime are used. Treatment does not shorten disease duration; reserve for complicated cases. Consultations Surgeon o Certain organisms cause abdominal pain and bloody stools.
Symptoms resembling appendicitis, hemorrhagic colitis, intussusception, or toxic megacolon may be appreciated. o If the infectious etiology in individuals with such symptoms is not certain, seek consultation with a surgeon. Infectious-disease specialist: Consider consultation with an infectious-disease specialist for any patient who is immunocompromised because of HIV infection, chemotherapy, or immunosuppressive drugs because atypical organisms are more likely, and complications can be more serious and fulminate.
Diet Breastfed infants with acute diarrhea should be continued on breast milk without any need for interruption. In fact, breastfeeding not only has a well-known protective effect against the development of enteritis, it also promotes faster recovery and provides improved nutrition. This is even more important in developing countries, where withdrawal of breastfeeding during diarrhea has been shown to have a deleterious effect on the development of dehydration in infants with acute watery diarrhea. Bananas, rice, applesauce, and toast diet o A banana, rice, applesauce, and toast (BRAT) diet was introduced in the United States in 1926 and has enjoyed vast popularity. However, no evidence shows that this diet is useful, and its poor protein content may be a contraindication; therefore, it is not recommended. o A strong body of evidence now suggests that resuming the prediarrhea diet is perfectly safe and must be encouraged, obviously respecting any (usually temporary) lack of appetite. Lactose ingestion o Although rotavirus can cause secondary transient lactose intolerance, this finding is believed to be generally not clinically relevant; use lactose-containing formulas in all individuals with diarrhea. o In an incident of worsening of diarrhea proven to be secondary to a clinically important lactose malabsorption in infants positive for rotavirus, a very transient use of lactose-free formulas (5-6 d) can be considered. Medication Summary Diarrheal diseases have been the object of numerous forms of treatment, both dietetic and pharmacologic, for centuries. However, the evidence is now clear that, in most cases, the best option for treatment of acute-onset diarrhea is the early use of oral rehydration therapy (ORT).[7] Pharmacological treatment is rarely of any use, and antidiarrheal drugs are often harmful. In terms of recommended antimicrobial treatment in the immunocompetent host, enteric bacterial and protozoan pathogens can be grouped as follows: Agents for whom antimicrobial therapy is always indicated: The consensus includes only V cholerae, Shigella species, and G lamblia. Agents for whom antimicrobial therapy is indicated only in selected circumstances, include the following: Infections by enteropathogenic E coli, when running a prolonged course Enteroinvasive E coli, based on the serologic, genetic, and pathogenic similarities with Shigella Yersinia infections in subjects with sickle cell disease Salmonella infections in very young infants, if febrile or with positive blood culture findings Probiotics Recently, some strains of probiotics (defined as live microorganisms that when ingested in adequate doses, provide a benefit to the host) have been found to be effective as an adjunct when treating children with acute diarrhea. Data from well-conducted randomized controlled trials on efficacy of probiotics in children with diarrhea are definitely positive. They consistently show a statistically significant benefit and moderate clinical benefit of a few, now well-identified probiotic strains (mostly Lactobacillus GG and Saccharomyces boulardii but also Lactobacillus reuteri) in the treatment of acute watery diarrhea (primarily rotaviral) in infants and young children in developed countries.
Such a beneficial effect seems to result in a reduction of the duration of diarrhea of about one day and seems to be exerted mostly on rotaviral diarrhea, with much less evidence of efficacy in invasive bacterial diarrhea. The effect is not only strain-dependent but also dose-dependent, with doses of at least 5 billion/d being required for effect.[10] Shortening the duration of diarrhea by one day may not appear to be hugely beneficial. However, in consideration of the high morbidity of the infection, even a reduction of this order is indeed desirable because it affords considerable savings in terms of loss of working days and direct health costs. Furthermore, probiotics may reduce the risk of spreading rotavirus infection by shortening diarrhea duration and volume of watery stool output and by reducing the fecal shedding of rotavirus, and they have been found useful in preventing the dissemination of hospital-acquired diarrheas. A recent position paper jointly published by the ESPGHAN and the European Society for Pediatric Infectious Disease (ESPID) stated, Probiotics may be an effective adjunct to the management of diarrhea. However, because there is no evidence of efficacy for many preparations, we suggest the use of probiotic strains with proven efficacy and in appropriate doses for the management of children with acute gastroenteritis as an adjunct to rehydration therapy (II, B). The following probiotics showed benefit in meta-analyses of randomized controlled trials: Lactobacillus GG (I, A) and S boulardii (II, B). Table 5 illustrates current assessment of the efficacy of probiotics in conditions characterized by diarrhea. Table 5. Probiotic Efficacy in Diarrhea (Open Table in a new window) Condition Patients and Most-Studied Probiotics Evidence of Controls Efficacy
(-
to
+++)
Prevention Diarrhea
of
Daycare 2000
Lactobacillus
GG +
Bifidobacterium
lactis
Lactobacillus
reuteri
Lactobacillus
casei
Bifidobacterium Streptococcus
bifidum + thermophilus
Prevention of Nosocomial 1000 Diarrhea Prevention of Antibiotic- 2000 Associated Diarrhea
Lactobacillus GG Lactobacillus
++ GG +++
Saccharomyces
boulardii
Infectious Diarrhea
3500
Lactobacillus
GG +++
Saccharomyces
boulardii
460 Lactobacillus GG + Persistent Diarrhea Antibiotic and antiparasitics agents Class Summary Antimicrobial agents, in addition to the immune system, help destroy offending organisms. Their use is confined to specific etiologies and/or clinical circumstances. Cefixime (Suprax) Potent long-acting oral cephalosporin with increased gram-negative coverage. Inhibits bacterial cell wall synthesis by binding to 1 or more PBPs. Bacteria eventually lyse because of ongoing activity of cell wall autolytic enzymes while cell wall assembly is arrested. Ceftriaxone (Rocephin) A third-generation cephalosporin antibiotic with activity against gram-positive and some gram-negative bacteria. Binds to PBPs, inhibiting bacterial cell wall growth. Cefotaxime (Claforan) Third-generation cephalosporin antibiotic with activity against gram-positive and some gram-negative bacteria. Binds to PBPs, inhibiting bacterial cell wall growth. Erythromycin (E.E.S., E-Mycin, Eryc, Ery-Tab, Erythrocin) Bacteriostatic macrolide with activity against most gram-positive organisms and atypical respiratory organisms. Useful for Campylobacter species and vibrio enteritis. Furazolidone (Furoxone) Antiparasitic agent with wide coverage. Nitrofuran with antiprotozoal activity. Alternative drug for children because availability in liquid suspension. Most common adverse effects are GI upset and brown discoloration of urine. Iodoquinol (Vytone, Yodoxin) Antiparasitic agents with wide coverage. Metronidazole (Flagyl) Very active against Giardia species, gram-negative anaerobes, and Entamoeba species. Imidazole ringbased antibiotic active against various anaerobic bacteria and protozoa. Often used in combination with other antimicrobial agents except for C difficile enterocolitis). Paromomycin (Humatin) Amebicidal and antibacterial aminoglycoside obtained from a strain of Streptomyces rimosus, active in intestinal amebiasis. Recommended for treatment of Diphyllobothrium latum, Taenia saginata, T solium, Dipylidium caninum, and Hymenolepis nana. Quinacrine (Atabrine) Very effective antiparasitic against Giardia species. Sulfamethoxazole and trimethoprim (Bactrim, Septra, Cotrim)
Folate-synthesis blocker with wide antibiotic coverage. Inhibits bacterial growth by inhibiting synthesis of dihydrofolic acid. Effective in E coli infections. Dosage form contains 5:1 ratio of sulfamethoxazole to trimethoprim. Vancomycin (Vancocin) Effective treatment (when PO) for antibiotic-associated colitis due to C difficile. However, reserve for individuals whose symptoms are not responding to less expensive and almost equally effective metronidazole. Tetracycline (Sumycin) Treats gram-positive and gram-negative organisms as well as mycoplasmal, chlamydial, and rickettsial infections. Good agent in older children who present with severe Yersinia species infection. Nitazoxanide (Alinia) Inhibits growth of C parvum sporozoites and oocysts and G lamblia trophozoites. Elicits antiprotozoal activity by interfering with pyruvate-ferredoxin oxidoreductase (PFOR) enzyme-dependent electron transfer reaction, which is essential to anaerobic energy metabolism. Available as a 20-mg/mL oral susp. Rifaximin (Xifaxan, RedActiv, Flonorm) Nonabsorbed (< 0.4%), broad-spectrum antibiotic specific for enteric pathogens of the gastrointestinal tract (ie, Gram-positive, Gram-negative, aerobic and anaerobic). Rifampin structural analog. Binds to beta-subunit of bacterial DNA-dependent RNA polymerase, thereby inhibiting RNA synthesis. Indicated for E coli (enterotoxigenic and enteroaggregative strains) associated with travelers' diarrhea. Vaccines Class Summary These agents elicit active immunization to increase resistance to infection. Vaccines consist of microorganisms or cellular components, which act as antigens. Administration of the vaccine stimulates the production of antibodies with specific protective properties. Rotavirus vaccine (RotaTeq, Rotarix) Currently, 2 PO administered live-virus vaccines are marketed in the United States. Both are indicated to prevent rotavirus gastroenteritis, a major cause of severe diarrhea in infants. RotaTeq is a pentavalent vaccine that contains 5 live reassortant rotaviruses and is administered as a 3dose regimen against G1, G2, G3, and G4 serotypes, the 4 most common rotavirus group A serotypes. It also contains attachment protein P1A (genotype P[8]). Rotarix protects against rotavirus gastroenteritis caused by G1, G3, G4, and G9 strains and is administered as a 2-dose series in infants aged 6-24 wk. Clinical trials found that the vaccines prevented 74-78% of all rotavirus gastroenteritis cases, nearly all severe rotavirus gastroenteritis cases, and nearly all hospitalizations. urther Inpatient Care Admit neonates or young infants with moderate dehydration, suspected infection with enterohemorrhagic E coli, or bloody diarrhea. Oral rehydration therapy (ORT) is the universally recommended form of treatment, proven to be successful even in children who vomit or have mild-to-moderate dehydration. Admit a child with severe dehydration. Also, ORT requires vigilance. If the caregiver cannot comply with protocol, consider admission. Further Outpatient Care Follow-up care depends on the severity of diarrhea and the child's age. Uncomplicated diarrhea in a school-aged child may not require follow-up care if the caregiver is reliable and has quick access to a physician. Closely monitor young children to ensure that complications do not occur. Closely monitor children who require labor-intensive ORT. Neonates require strict follow-up care within a few days of illness to ensure that malabsorption and dehydration do not occur. Deterrence/Prevention Vaccines are indicated for persons with high risk of exposure to some pathogens. In February 2006, the United States Food and Drug Administration (FDA) approved an oral vaccine for rotavirus (RotaTeq). Soon thereafter, the AAP and the Advisory Committee on
Immunization Practices (ACIP) recommended RotaTeq to be part of regularly scheduled childhood immunizations. RotaTeq is administered in a 3-dose series starting between age 6-12 weeks and completing before 32 weeks. An older rotavirus vaccine (RotaShield) was associated with an increased incidence of intussusception and is no longer on the market, but RotaTeq did not show an increased risk compared with placebo in clinical trials. In April 2008, the FDA approved Rotarix, another oral vaccine, for prevention of rotavirus gastroenteritis. The current recommendation is to administer 2 separate doses of Rotarix to patients aged 6-24 weeks. Rotarix was efficacious in a large study, which reported that Rotarix protected patients with severe rotavirus gastroenteritis and decreased the rate of severe diarrhea or gastroenteritis of any cause.[11] A study that involved over 63,000 patients who received Rotarix or placebo at age 2 months and at age 4 months reported a decreased risk of intussusception in patients who received Rotarix. [11] The intussusception data was determined over a 31-day observation period (inpatient or outpatient) after each dose of the Rotarix vaccine; this also included a 100-day surveillance period for all serious adverse events. Although more patients who received Rotarix were observed to have seizures or pneumonia-related deaths, this link has not been directly established to Rotarix. However, on March 22, 2010, the FDA recommended the temporary discontinuation of its use, pending further studies on the reported presence of an apparently benign pig virus in the Rotarix vaccine. A Cochrane Database review evaluated the results of 43 trials with 190,551 participants comparing rotavirus vaccines, both the monovalent and pentavalent types (RV1 and RV5), with placebo. Both vaccines were found to be effective in preventing rotavirus diarrhea.[12] The Salmonella typhi vaccine is recommended for travelers to countries with a high risk of this infection, persons with intimate exposure to a documented typhoid fever carrier, and workers with frequent exposure to this bacteria. Live-attenuated, killed whole-cell, and capsular polysaccharide vaccines are available. The Vibrio species vaccine is available but only protects 50% of immunized persons for 3-6 months. It is not indicated for use. Complications Common complications include the following: Aeromonas caviae - Intussusception, gram-negative sepsis, hemolytic-uremic syndrome (HUS) Campylobacter species -Bacteremia, meningitis, cholecystitis, urinary tract infection, pancreatitis, Reiter syndrome (RS) C difficile - Chronic diarrhea C perfringens serotype C - Enteritis necroticans Enterohemorrhagic E coli - Hemorrhagic colitis Enterohemorrhagic E coli O157:H7 - HUS Plesiomonas species - Septicemia Salmonella species - Seizures, HUS, perforation, RS Vibrio species - Rapid dehydration Y enterocolitica - Appendicitis, perforation, intussusception, peritonitis, toxic megacolon, cholangitis, bacteremia, RS Rotavirus - Isotonic dehydration, carbohydrate intolerance Giardia species - Chronic fat malabsorption Cryptosporidium species - Chronic diarrhea Entamoeba species - Colonic perforation, liver abscess Enteric fever is caused by S typhi. This syndrome has an insidious onset of malaise, fever, abdominal pain, and bradycardia. Diarrhea and rash (rose spots) appear after 1 week of symptoms. Bacteria may have disseminated at that time, and treatment is required to prevent systemic complications such as hepatitis, myocarditis, cholecystitis, or GI bleeding.
HUS is caused by damage to vascular endothelial cells by verotoxin (released by enterohemorrhagic E coli and by Shigella organisms). Thrombocytopenia, microangiopathic hemolytic anemia, and acute renal failure characterize HUS. Symptoms usually develop one week after onset of diarrhea, when the organism may be absent. RS can complicate acute infections and is characterized by arthritis, urethritis, conjunctivitis, and mucocutaneous lesions. Individuals with RS usually do not demonstrate all features. Carrier states are observed after some bacterial infections. After diarrhea caused by Salmonella organisms, 1-4% of individuals with nontyphoid and enteric fever infections become carriers. The carrier stage for Salmonella organisms is more likely for females, infants, and individuals with biliary tract disease. Asymptomatic C difficile carriage may be observed in as many as 20% of hospitalized patients receiving antibiotics and in 50% of infants. Rotavirus is excreted asymptomatically in feces of children who were previously infected, typically for as long as 1-2 weeks. Prognosis In developed countries, with proper management, prognosis is very good. However, data show an increase in diarrhea-associated deaths among US children from the mid-1980s through 2006. During 2005-2007, 1087 diarrhea-associated infant deaths were reported with 86% of deaths occurring among low birthweight (< 2500g) infants. Risk factors for these infants included male sex, black race, and low 5minute Apgar score (< 7).[5] Death is caused predominantly by dehydration and secondary malnutrition from a protracted course. Severe dehydration must be managed with parenteral fluids. Once malnutrition from secondary malabsorption begins, prognosis turns grim unless the patient is hospitalized and supplemental parenteral nutrition is started. Neonates and young infants are at particular risk of dehydration, malnutrition, and malabsorption syndromes. Even though the mortality rate is low in developed countries, children can die from complications; however, prognosis for children in countries without modern medical care and children with comorbid conditions is more guarded. Patient Education Education is most important for prevention and treatment. Proper ORT prevents dehydration, and early refeeding speeds recovery of intestinal mucosa. With caregiver, emphasize proper hygiene and food preparation practices to prevent future infections and spread.
También podría gustarte
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceCalificación: 4 de 5 estrellas4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeCalificación: 4 de 5 estrellas4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe EverandShoe Dog: A Memoir by the Creator of NikeCalificación: 4.5 de 5 estrellas4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe EverandGrit: The Power of Passion and PerseveranceCalificación: 4 de 5 estrellas4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Calificación: 4 de 5 estrellas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe EverandThe Little Book of Hygge: Danish Secrets to Happy LivingCalificación: 3.5 de 5 estrellas3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe EverandNever Split the Difference: Negotiating As If Your Life Depended On ItCalificación: 4.5 de 5 estrellas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureCalificación: 4.5 de 5 estrellas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryCalificación: 3.5 de 5 estrellas3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDe EverandRise of ISIS: A Threat We Can't IgnoreCalificación: 3.5 de 5 estrellas3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDe EverandThe Emperor of All Maladies: A Biography of CancerCalificación: 4.5 de 5 estrellas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaCalificación: 4.5 de 5 estrellas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersCalificación: 4.5 de 5 estrellas4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDe EverandOn Fire: The (Burning) Case for a Green New DealCalificación: 4 de 5 estrellas4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyCalificación: 3.5 de 5 estrellas3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDe EverandTeam of Rivals: The Political Genius of Abraham LincolnCalificación: 4.5 de 5 estrellas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe EverandThe Unwinding: An Inner History of the New AmericaCalificación: 4 de 5 estrellas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreCalificación: 4 de 5 estrellas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Calificación: 4.5 de 5 estrellas4.5/5 (121)
- The Perks of Being a WallflowerDe EverandThe Perks of Being a WallflowerCalificación: 4.5 de 5 estrellas4.5/5 (2104)
- Her Body and Other Parties: StoriesDe EverandHer Body and Other Parties: StoriesCalificación: 4 de 5 estrellas4/5 (821)
- Home Visit PlanDocumento2 páginasHome Visit Planako at ang exoAún no hay calificaciones
- ThesisDocumento95 páginasThesisDrGeorge Saad AbdallaAún no hay calificaciones
- Package Insert - Varivax (Refrigerator)Documento14 páginasPackage Insert - Varivax (Refrigerator)Jose Eduardo Oliva MarinAún no hay calificaciones
- Health Grade10 4th QuarterDocumento40 páginasHealth Grade10 4th QuarterYnjel HilarioAún no hay calificaciones
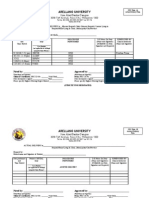
- Arellano University: Jose Abad Santos CampusDocumento7 páginasArellano University: Jose Abad Santos CampusLloyd VargasAún no hay calificaciones
- Analisis Lama Waktu Pelayanan Laboratorium Di Rumah Sakit Umum Daerah Pasaman BaratDocumento8 páginasAnalisis Lama Waktu Pelayanan Laboratorium Di Rumah Sakit Umum Daerah Pasaman Baratdina filanAún no hay calificaciones
- Oct Symp AbhiDocumento54 páginasOct Symp AbhiMonisha ArulalanAún no hay calificaciones
- CKDDocumento35 páginasCKDgailAún no hay calificaciones
- Endocrine PancreasDocumento21 páginasEndocrine Pancreaslacafey741Aún no hay calificaciones
- Antimicrobial Effect of Aqueous Banana Peel Extract, IraqDocumento4 páginasAntimicrobial Effect of Aqueous Banana Peel Extract, IraqLilis KhusnulAún no hay calificaciones
- Pharmacology Test 1Documento39 páginasPharmacology Test 1Niki BolinAún no hay calificaciones
- Clinical Handbook of Insomnia (2017)Documento292 páginasClinical Handbook of Insomnia (2017)jcholguin.conciencia4100100% (7)
- OET Reading Test 7 - Part BDocumento13 páginasOET Reading Test 7 - Part BLOTSOFTESTS80% (5)
- The Sketch of Indonesia Medicine: Sugma AP, MD, MARSDocumento42 páginasThe Sketch of Indonesia Medicine: Sugma AP, MD, MARSRaja Friska YulandaAún no hay calificaciones
- Midterm Exam 1Documento6 páginasMidterm Exam 1Joanne Bernadette AguilarAún no hay calificaciones
- Chapter 1: Introduction To Operative DentistryDocumento11 páginasChapter 1: Introduction To Operative DentistryMariam AdnanAún no hay calificaciones
- Colchicine Drug Study For Gouty ArthritisDocumento3 páginasColchicine Drug Study For Gouty ArthritisLeslie PaguioAún no hay calificaciones
- New India Cancer Guard FinalDocumento28 páginasNew India Cancer Guard FinalumapAún no hay calificaciones
- (S-W5-Sun-Gen.S) (By Dr. Emad) Gall Bladder 1Documento28 páginas(S-W5-Sun-Gen.S) (By Dr. Emad) Gall Bladder 1Haider Nadhem AL-rubaiAún no hay calificaciones
- Breast Cancer - DZMEDocumento6 páginasBreast Cancer - DZMEMarife CompraAún no hay calificaciones
- CLUBFOOT GuidelineDocumento111 páginasCLUBFOOT GuidelineNuhiat NahreenAún no hay calificaciones
- Evaluasi Usg Dan Tatalaksana Pada Varises Vena Tungkai - DR RamziDocumento31 páginasEvaluasi Usg Dan Tatalaksana Pada Varises Vena Tungkai - DR RamziMohamad ZulfikarAún no hay calificaciones
- Risk For Infection Related To Presence of Surgical Wounds As Evidenced by MER 2nd DegreeDocumento3 páginasRisk For Infection Related To Presence of Surgical Wounds As Evidenced by MER 2nd DegreeSenyorita KHaye75% (12)
- Veterinary Pharmacology 2011Documento35 páginasVeterinary Pharmacology 2011Satnam singhAún no hay calificaciones
- بنك الأسئلةDocumento775 páginasبنك الأسئلةسماح صلاح100% (1)
- FC Derm (SA) Regulations 26-3-2014Documento13 páginasFC Derm (SA) Regulations 26-3-2014matentenAún no hay calificaciones
- By: Abduljabbar Hamid Jabbar: University of Baghdad-College of Medicine M. B. Ch. BDocumento14 páginasBy: Abduljabbar Hamid Jabbar: University of Baghdad-College of Medicine M. B. Ch. BXena XenaAún no hay calificaciones
- Malabsorption SyndromeDocumento7 páginasMalabsorption SyndromeHassan.shehri100% (4)
- Buku Panduan Mahasiswa Blok 11 2021-2022 (Kurikulum 2012) - 25-34Documento10 páginasBuku Panduan Mahasiswa Blok 11 2021-2022 (Kurikulum 2012) - 25-34Qonita AztAún no hay calificaciones
- Opalescence Tooth Whitening Systems: At-Home Whitening InstructionsDocumento1 páginaOpalescence Tooth Whitening Systems: At-Home Whitening InstructionsPande NandaAún no hay calificaciones