Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Exam 2 Study Guide - Cellular Response To Injury
Cargado por
Wendy SuhDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Exam 2 Study Guide - Cellular Response To Injury
Cargado por
Wendy SuhCopyright:
Formatos disponibles
MOUNT ST.
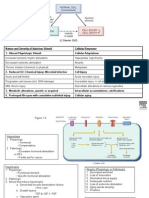
MARYS COLLEGE DEPARTMENT OF NURSING NURSING 54/44A INTRODUCTION TO PATHOPHYSIOLOGY Study Guide for CELLULAR RESPONSE TO INJURY I. Concept of Cellular injury: A. Significance of discussing cellular injury *GOAL: -Permit survival -Maintain cell function B. Outcome of cell injury see Figure 5-8 in Porth 1. Reversible cellular injury- cell recovery & return to normal function. 2 results are: - cellular swelling (due to impairment of Na+/k+ pump, there is an increase of Na+ in the cell which causes swelling & leads to hypoxic cell injury) - fatty change (due to an increased fat load or the inability of a damaged cell to metabolize Fat) 2. Programmed cell death (a.k.a.- APOPTOSIS). Programmed to remove injured and worn out cells; Controls tissue regeneration. 3. Cell death and necrosis Occurs in irreversible damaged cells; Refers to cell death in an organ or tissue that is still part of a living organism. (Example: GANGRENE); Necrosis often interferes with cell replacement and tissue regeneration *Necrosis undergoes 3 pathways: -Liquefaction (solid tissue fluid or semi fluid state) -Coagulation (clumping together due to protein denaturation. HEAT plays an important role) -Caseous (dead cells that become cheese-like debris) II. Cellular adaptation: A. Atrophy- a DECREASE in cell size due to a decrease in work demand; as cells become smaller reduce their O2 consumption which can lead to hypoxia; when a sufficient amount of cells are involved, the entire muscle or tissue atrophies. *5 Causes of ATROPHY are: - Disuse (when there is a reduction in skeletal muscle use; Example: when muscle of an extremity is in a cast, it becomes smaller because it is not being
used; but muscle size can be restored when cast is removed and muscle use is resumed) - Denervation (loss of nerves = loss of electrical impulses; occurs in muscles of paralyzed limbs - Loss of Endocrine stimulation (a type of disuse atrophy; in women loss of estrogen stimulation during menopause casue atrophic changes in reproductive system) - Inadequate nutrition (cells not getting enough energy) - Ischemia/ blood flow (leads to decreased O2 of the cells which can lead to necrosis/cell death.) B. Hypertrophy- an INCREASE in cell size due to an increased workload or increased stimulation of growth hormone Commonly seen in Cardiac & Skeletal cells Exercise is an example of Physiologic Hypertrophy Pathologic Hypertrophy occurs as a result of disease ATP Depletion initializes Hypertrophic process!! (cells are not getting enough nutrients for energy so muscle begins to HYPERTROPHY)
C. Hyperplasia- is an increase in the number of cells in an organ or tissue - It occurs with cells that are capable of mitotic division such as: Epidermis, Intestinal epithelium. Glandular tissue It is a controlled process that occurs in response to a stimulus and ceases after the stimulus has been removed. Although HYPERTROPHY and HYPERPLASIA are two distinct processes, they may occur together and are often triggered by the same mechanism.
D. Metaplasia- Reversible Change- in which one adult cell type is replaced by another adult cell type. usually occurs as a result of chronic inflammation and irritation and allows for a better substitution of cells that are better able to survive Example would be: substitution of Stratified squamous epithelium for Ciliated columnar epithelium in the trachea and large airways of a habitual SMOKER.
E. Dysplasia- deranged cell growth; results in abnormal changes in size, shape, structure; can be found in epithelium of respiratory tract or cervix. Although it is abnormal, it is adaptive in that it is potentially Reversible after the irritating cause has been removed. Dysplasia is strongly implicated as precursor of Cancer, however it does not necessarily lead to cancer. F. Intracellular accumulations- represent a build up of substances that the body cannot immediate use or eliminate. These substances may accumulate in the cytoplasm or nucleus. These substances can be classified into 3 groups: - normal substances: carbs, proteins, lipids abnormal endogenous sunstances: those resulting from inbron errors of metabolism (LIVER will become Endogenous and Fatty if it does not metabolize/break down substances working so hard that it becomes fatty and leads to CIRRHOSIS) exogenous substances: environmental agents and pigments that cannot be broken down by the cell; may be harmless or in some cases toxic. Example: CARBON (can blacken the lung and cause lung disease)
G. Pathologic calcifications abnormal deposition of calcium salts with smaller amounts of Magnesium, Iron and other Minerals -Dystrophic calcification: occurs in injured or dying/dead tissue; commonly seen in Atherosclerosis aorta, blood vessels and damaged heart valves. **Leads to Organ Dysfunction** **Example: Calcification of aortic valve leads to aortic stenosis in elderly** -Metastatic calcification: in the media of the arteries; occurs in normal tissues as a result of increased Calcium levels (HYPERCALCEMIA) III. Cellular injury A. Major causes of cellular injury 1. Injury from physical agentsmechanical forces- body impact with another object (tear tissue, obstruct blood vessels, impair blood flow, fracture bones) extreme temperatures- cause damage to cells & their organelles (burns, severe heat stroke, frostbite, hyperthermia)- exposure to cold can cause Vasoconstriction and decrease blood flow and lead to Hypoxic tissue injury; with more intense HEAT, coagulation occurs.
electrical injury- cause severe tissue injury and disrupts cardiac (heart) & neural (brain) impulses- electrical energy turns to heat which is why tissue damage by electrical injuries is caused by heat production in the tissues. 2. Radiation injuryIonizing radiation- radiation energy above the UV range (X-rays, electromagnetic)- can damage DNA and CYTOPLASM and lead to organ dysfunction Ultraviolet radiation- (UV rays, Sun)- UV rays also damage DNA; Can cause sunburn and increases the risk of skin cancer; We need sunlight to metabolize Vitamin D, but too much can lead to abnormalities (such as skin cancer); degree of risk depends on the type of UV rays and the intensity of the exposure Non-Ionizing radiation- (Infrared light, Ultrasound, Microwaves, Laser energy)- All this energy is converted to thermal energy. Injury from these sources tend to involve DERMAL and SUBCUTANEOUS tissue injury. 3. Chemical injury- chemical agents can injure the cell membrane and other structures, block enzymatic pathways, coagulate proteins - Air & water pollution - Tobacco smoke - Processed & Preserved foods - Drugs & Alcohol (can directly or indirectly damage tissues) Acetaminophen: a common over the counter drug that is detoxified by the liver; when large amounts are ingested, it becomes toxic, causing liver necrosis. Alcohol: large and persistent amount can cause Cirrhosis of the liver - Heavy metals (Lead & Mercury) - Carbon Monoxide (this is not good because cell wont bing to oxygen anymore which leads to ischemia and eventually necrosis) 4. Injury from biologic agents- able to replicate & produce injurious effect (Viruses) - Viruses - Bacteria - Rickettsiae - Mycoplasms - Fungi - Protozoa 5. Genetic derangements can cause metabolic disturbances & an altered immune response 6. Injury from nutritional imbalances- Undernutrition &
Overnutrition Undernutrition: unable to meet the metabolic needs of the cell **Dietary deficiency can occur in the form of starvation, in which there is a deficiency of all nutrients & vitamins. Starvation can cause widespread tissue damage** Overnutrition: more than the body needs or requires; excess makes the cells work harder
**OBESITY & diets hugh in saturated fats can predispose a person to atherosclerosis** B. Mechanisms of cell injury 1. Free radical injury- when a molecule has an unpaired electron that causes it to be unstable & highly reactive. When cells are susceptible, Free Radicals can take over. The actions of Free Radicals may damage cells and tissues 2. Hypoxic cell injury- Hypoxia deprives the cell of oxygen (Hypoxia O2 deficiency leads to ischemia then Necrosis/Cell death) we see this with MI (heart attack); It can also result from inadequate oxygen in the air (Ex: @ High Altitudes) Some cells, such as those of the BRAIN, HEART & KIDNEY, require large amounts of Oygen. Brain cells begin to undergo permanent damage after 4-6 minutes of No Oxygen *Causes of Hypoxia: - DECREASED blood supply to the area - DECREASED oxygen carrying capacity of blood - Ventilation Perfusion (mismatch; unable to transfer O2 & CO) - DECREASED O2 in the air 3. Impaired calcium homeostasis- normally, Intracellular Ca+ levels are kept lower compared with Extracellular levels; The Increased Ca+ level may inappropriately activate a number of enzymes with potentially damaging effects. (**In our notes, ATP depletion is also mentioned**) C. Responses/ results of reversible cell injury 1. Cellular swelling- caused by impairment of Na+/K+ membrane pump; This causes increased K+ levels and Increased Na+ into the cell (with water following) and results in hypoxic cell injury
2. Fatty cellular changes Fat is dispersed in cytoplasm; usually an indication of severe injury; may occur from an increased Fat load or the inability of injured cells to metabolize fat properly. D. Cell death and necrosis 1. Apoptosis- Programmed Cell Death- (Normal cell deletion & Renewal) programmed to remove injured or worn out cells; controlled tissue regeneration 2. Necrosis- refers to cell death in an organ or tissue that is still part of a living organism (ex: GANGRENE); necrosis interferes with cell replacement & tissue regeneration 3. Types of necrosis a. Liquefaction- conversion of solid tissues to fluid or semi-fluid state. Some cells die, but enzymes are not destroyed. b. Coagulation Most common type!- characteristic of hypoxic injury; Clumping together due to protein denaturation; HEAT plays an important role (it Denatures) c. Caseous- dead cells that become soft- cheese like debris (Soft & Granular) d. Gangrene- when a considerable amount of tissue undergoes necrosis. Can be classified as: - Dry Gangrene: the part becomes dry and shrinks, the skin wrinkles and its color changes to dark brown or black. The spread of dry gangrene is slow; ususally results from interference with Arterial Blood Supply. Wet/Moist Gangrene: the area is cold, swollen and pulseless; the skin is moist and black; the spread of tissue damage is rapid; it results from interference with Venous Return; it is Smelly and has a foul odor; Moist Gangrene may affect internal organs or the extremities unlike Dry Gangrene that is confined exclusively to the extremity. Bacterial invasion plays a HUGE role Gas Gangrene: a serious and potentially fatal disease (gas forming microorganism); caused by Clostridium Bacteria; amputation may be required to prevent spread Diabetic Gangrene: result of neuropathy nerve-endings; Feet is an important teaching with diabetes (diabetic neuropathy cant feel cuts or other things on feet)
IV. Cellular, tissue, and systemic aging A. Cellular basis of aging - normal physiologic process - not considered a disease
gradual result of wear-and-tear
B. Theories of Aging 1. Stochastic: aging as a result of lifelong genetic damage; Accumulations of lifelong random injuries and events 2. Nonstochastic: aging results from genetically controlled developmental program, or built in self-destructive processes C. Physiologic Changes of Aging 1. Atrophy- cells/tissue decrease in size 2. Sclerosis- thickening or hardening of organ or tissues 3. Decrease in organ functions- Lungs (lung capacity diminishes w/ age) - GI - GU (problems with incontinence) 4. No replacement of permanent cells 5. Decrease adaptation to stress- the older you get, the less adaptation to stress you get
También podría gustarte
- 120-Nr-M.D. Degree Examination - June, 2008-Pathology-Paper-IDocumento16 páginas120-Nr-M.D. Degree Examination - June, 2008-Pathology-Paper-IdubaisrinivasuluAún no hay calificaciones
- Cirrhosis Jol 2009Documento54 páginasCirrhosis Jol 2009SaaraAlleyahAlAnazi100% (1)
- MCQ Sample QuestionsDocumento4 páginasMCQ Sample QuestionsNaveen Vachipalli100% (1)
- Base (Path Anatomy) 2014 FIRSTDocumento39 páginasBase (Path Anatomy) 2014 FIRSTHarsh NimavatAún no hay calificaciones
- PATHOLOGY Mendelian DisordersDocumento8 páginasPATHOLOGY Mendelian DisordersAmna BaigAún no hay calificaciones
- Fatty Liver (1) - General PathologyDocumento22 páginasFatty Liver (1) - General PathologyDarien LiewAún no hay calificaciones
- Chapter 21 Lippincott BiochemistryDocumento53 páginasChapter 21 Lippincott BiochemistryMeysam SajjadiAún no hay calificaciones
- Robinson Pathology Chapter 20 KidneyDocumento11 páginasRobinson Pathology Chapter 20 KidneyElina Drits100% (1)
- 07 Pathological ClacificationDocumento10 páginas07 Pathological Clacificationraanja2Aún no hay calificaciones
- Cell Injury Notes-1Documento63 páginasCell Injury Notes-1Stefanie VirniaAún no hay calificaciones
- Lecture 3 - The Cell and Reaction To Injury - 2 Sep 2006Documento19 páginasLecture 3 - The Cell and Reaction To Injury - 2 Sep 2006api-3703352Aún no hay calificaciones
- Microb Seminar Group 3 (LATEST)Documento21 páginasMicrob Seminar Group 3 (LATEST)HasifAún no hay calificaciones
- The SkinDocumento4 páginasThe SkinDella Ayu PutriAún no hay calificaciones
- Robbins Chapter 1 DiagramsDocumento18 páginasRobbins Chapter 1 DiagramsYoja GarzonAún no hay calificaciones
- Chapter 23 Lippincott BiochemistryDocumento44 páginasChapter 23 Lippincott BiochemistryMeysam SajjadiAún no hay calificaciones
- KROK Part - II PDFDocumento99 páginasKROK Part - II PDFPiravi 19Aún no hay calificaciones
- The Liver: Dr. I Made Naris Pujawan, M.Biomed, SP - PADocumento19 páginasThe Liver: Dr. I Made Naris Pujawan, M.Biomed, SP - PAAnonymous D29e00Aún no hay calificaciones
- 03 Cell InjuryDocumento72 páginas03 Cell InjuryLunaLure100% (1)
- Cell Types: Superficial CellsDocumento7 páginasCell Types: Superficial Cellsთამარ ჩალაურიAún no hay calificaciones
- CHAPTER 35 AntigensAgglutinogensDocumento2 páginasCHAPTER 35 AntigensAgglutinogensg_komolafe100% (1)
- Genetic Basis of Disease PMDocumento79 páginasGenetic Basis of Disease PMsunday daniel100% (1)
- Path Anat Part 1Documento184 páginasPath Anat Part 1Javier Saad100% (1)
- Important QuestionsDocumento31 páginasImportant QuestionssandeepAún no hay calificaciones
- General Reactions Involved in Amino Acid Metabolism: Dr. Dhiraj J TrivediDocumento32 páginasGeneral Reactions Involved in Amino Acid Metabolism: Dr. Dhiraj J Trivediendale gebregzabherAún no hay calificaciones
- Treatment of Hemostasis DisordersDocumento17 páginasTreatment of Hemostasis DisordersDiana HyltonAún no hay calificaciones
- Medical Pathology Ii. Pathology of Urinary System Lectuer NotesDocumento26 páginasMedical Pathology Ii. Pathology of Urinary System Lectuer Noteseric epahAún no hay calificaciones
- Atherosclerosis 1Documento45 páginasAtherosclerosis 1MoonAIRAún no hay calificaciones
- Oncology Questions by DR - OkashaDocumento31 páginasOncology Questions by DR - Okashamohammed okashaAún no hay calificaciones
- Apoptosis PPT, Pathological AnatomyDocumento15 páginasApoptosis PPT, Pathological AnatomyN J3 CAún no hay calificaciones
- Thesis of Dr. AKM Maruf Raza PDFDocumento95 páginasThesis of Dr. AKM Maruf Raza PDFMaruf Raza DarubagiAún no hay calificaciones
- CHR InflammationDocumento33 páginasCHR InflammationAlnzeer6Aún no hay calificaciones
- Oxford McqsDocumento15 páginasOxford McqsaliaaAún no hay calificaciones
- For More Details Please Visit Our WebsiteDocumento25 páginasFor More Details Please Visit Our Websiteajie354Aún no hay calificaciones
- Pathophysiology ControlTest-1 For 3rd Yr ZSMUDocumento9 páginasPathophysiology ControlTest-1 For 3rd Yr ZSMUDrRaghavender ReddyAún no hay calificaciones
- Kinds of Blood CellDocumento3 páginasKinds of Blood CellBalkis HumairohAún no hay calificaciones
- Presented by T. V. L. Sahithi Ist Year PG Dept of PeriodonticsDocumento49 páginasPresented by T. V. L. Sahithi Ist Year PG Dept of Periodonticslakshmi sahithi natakalaAún no hay calificaciones
- Congo Red and AnaloguesDocumento38 páginasCongo Red and AnaloguesShervin Mortazavi100% (1)
- Blood and Tissue ProtozoaDocumento32 páginasBlood and Tissue ProtozoaFort SalvadorAún no hay calificaciones
- Disorders of Cell Growth & NeoplasiaDocumento62 páginasDisorders of Cell Growth & NeoplasiaPrakash PanthiAún no hay calificaciones
- Urinary Tract ReviewDocumento12 páginasUrinary Tract ReviewJessica MooreAún no hay calificaciones
- Genetics-Exam 4 1Documento5 páginasGenetics-Exam 4 1Farhan Ahmed100% (1)
- Robbins Ch. 19 The Pancreas Review QuestionsDocumento3 páginasRobbins Ch. 19 The Pancreas Review QuestionsPA2014100% (1)
- Systemic Response To InjuryDocumento45 páginasSystemic Response To InjuryAbdulaziz Al-Akhras100% (1)
- Ilovepdf Merged PDFDocumento177 páginasIlovepdf Merged PDFNishankumar JhaAún no hay calificaciones
- Chapter 13 Neoplastic Proliferations of White CellsDocumento16 páginasChapter 13 Neoplastic Proliferations of White CellsOmar100% (1)
- Anatomy and Pathology of Testicular Tumors - UpToDateDocumento26 páginasAnatomy and Pathology of Testicular Tumors - UpToDateBhargav YagnikAún no hay calificaciones
- Neuropathology: FK UisuDocumento28 páginasNeuropathology: FK UisuAnggi WahyuAún no hay calificaciones
- Krok 1anatomy2Documento1 páginaKrok 1anatomy2Sandeep KumarAún no hay calificaciones
- EmfizemulDocumento19 páginasEmfizemulMirela IoanaAún no hay calificaciones
- Pat An AnewDocumento126 páginasPat An AnewgshchurovskiyAún no hay calificaciones
- NUS LSM4232 Lecture NotesDocumento40 páginasNUS LSM4232 Lecture Notesijclement07Aún no hay calificaciones
- @PIDs Curs 200903Documento43 páginas@PIDs Curs 200903Mohammad_Islam87Aún no hay calificaciones
- Granulomatous Inflammation ThyroidDocumento55 páginasGranulomatous Inflammation ThyroidKamlesh PrajapatiAún no hay calificaciones
- Immune ToleranceDocumento7 páginasImmune TolerancehamaadaAún no hay calificaciones
- FBC Interpretation and Function of Blood ComponentsDocumento7 páginasFBC Interpretation and Function of Blood ComponentsFrancesca LiAún no hay calificaciones
- General Pathology QuizDocumento2 páginasGeneral Pathology QuizMatt DickoAún no hay calificaciones
- Lung AbcessDocumento12 páginasLung AbcessABI OFFICIALAún no hay calificaciones
- Test 3 Study Guide INNATE DEFENSES A&P2Documento13 páginasTest 3 Study Guide INNATE DEFENSES A&P2Sarah C. SnooksAún no hay calificaciones
- Selected Topics in the History of Biochemistry. Personal Recollections. Part IIIDe EverandSelected Topics in the History of Biochemistry. Personal Recollections. Part IIICalificación: 1 de 5 estrellas1/5 (1)
- Chapman System of ClassificationDocumento6 páginasChapman System of Classificationvineetvishal73Aún no hay calificaciones
- Life Sciences Grade 10 Learner Support DocumentDocumento36 páginasLife Sciences Grade 10 Learner Support DocumentLiezel100% (1)
- Science 9 Quarter 1 Week 3 Sim 4Documento17 páginasScience 9 Quarter 1 Week 3 Sim 4Rodel CamposoAún no hay calificaciones
- Week 5 G7Documento3 páginasWeek 5 G7Mary Grace del RosarioAún no hay calificaciones
- Module 2 Gen Bio CellsDocumento59 páginasModule 2 Gen Bio CellsSophia Joy A. FajardoAún no hay calificaciones
- Hypoxia: Hypoxic Injury To CellsDocumento5 páginasHypoxia: Hypoxic Injury To CellsUloko ChristopherAún no hay calificaciones
- Click: Cambridge IGCSE Biology Extended LevelDocumento20 páginasClick: Cambridge IGCSE Biology Extended Levelkaziba stephenAún no hay calificaciones
- Basics of Medical Microbiology & ParasitologyDocumento25 páginasBasics of Medical Microbiology & ParasitologyJustine Val RevalidaAún no hay calificaciones
- Continuity of Life & Genetic ControlDocumento25 páginasContinuity of Life & Genetic ControlYudi Santoso0% (1)
- Birla Institute of Technology and Science, Pilani: Hyderabad CampusDocumento3 páginasBirla Institute of Technology and Science, Pilani: Hyderabad CampuspranavjibhakateAún no hay calificaciones
- General Biology QuizDocumento2 páginasGeneral Biology QuizQueng ElediaAún no hay calificaciones
- Peter Gariaev An Open Letter From The Father of WavegeneticsDocumento3 páginasPeter Gariaev An Open Letter From The Father of WavegeneticsRafael Gonzalez100% (1)
- General Biology 1 Module 2Documento16 páginasGeneral Biology 1 Module 2Ennyliejor YusayAún no hay calificaciones
- 1 General Biology 1 - IntroductionDocumento6 páginas1 General Biology 1 - IntroductionKay JusonAún no hay calificaciones
- Lesson 1 Cells The Building Blocks of LifeDocumento15 páginasLesson 1 Cells The Building Blocks of LifeGwen MarielleAún no hay calificaciones
- Human and Social Biology SyllabusDocumento132 páginasHuman and Social Biology Syllabussmbdy tbhhhAún no hay calificaciones
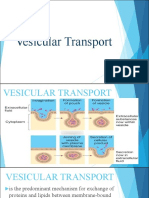
- Vesicular Transport (Group 3)Documento30 páginasVesicular Transport (Group 3)Joanna RollanAún no hay calificaciones
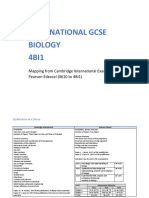
- Cambridge - Igcse.biology - Mapped.against - Edexcel.ig FinalDocumento86 páginasCambridge - Igcse.biology - Mapped.against - Edexcel.ig FinalBenish RehanAún no hay calificaciones
- Sankalp Sanjeevni Neet: BiologyDocumento13 páginasSankalp Sanjeevni Neet: BiologyKey RavenAún no hay calificaciones
- 9700 w18 QP 21 PDFDocumento16 páginas9700 w18 QP 21 PDFNoor HannyAún no hay calificaciones
- Esempio Di Prova English TOLC-FDocumento32 páginasEsempio Di Prova English TOLC-FAhlam Morjani100% (2)
- Visible Biology Site License Lab Activities Prokaryotic and Eukaryotic Cells StudentDocumento13 páginasVisible Biology Site License Lab Activities Prokaryotic and Eukaryotic Cells StudentALEXANDRE RAFAEL KUREKAún no hay calificaciones
- Biology of Sars-Cov-2Documento5 páginasBiology of Sars-Cov-2Nicole Sanchez100% (1)
- HES 032 - SAS 1 - Merged-1Documento1 páginaHES 032 - SAS 1 - Merged-1bangtanswifue -Aún no hay calificaciones
- Mader/Biology, 10/e - Chapter Outlines: 1.1 How To Define LifeDocumento363 páginasMader/Biology, 10/e - Chapter Outlines: 1.1 How To Define LifeAli AshrafAún no hay calificaciones
- Transwell Permeable Supports: Including Snapwell and Netwell InsertsDocumento8 páginasTranswell Permeable Supports: Including Snapwell and Netwell InsertsPili CárdenasAún no hay calificaciones
- CellDocumento33 páginasCellbrij100% (1)
- Grade 3 Vocabulary Expander Writing Workbook PDFDocumento39 páginasGrade 3 Vocabulary Expander Writing Workbook PDFJasmin Manio100% (1)
- Mira Nuri Santika 1811040002 Tugas ListeningDocumento2 páginasMira Nuri Santika 1811040002 Tugas ListeningMira NurisantikaAún no hay calificaciones
- Naked Mole Rat SlidesDocumento57 páginasNaked Mole Rat SlidesSharmila JeromeAún no hay calificaciones