Documentos de Académico
Documentos de Profesional
Documentos de Cultura
Ebcpg Colonic Injuries
Cargado por
pot_domingoDescripción original:
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
Ebcpg Colonic Injuries
Cargado por
pot_domingoCopyright:
Formatos disponibles
Evidence-based Clinical Practice Guidelines Management of Penetrating Colonic Injuries
on
the
Operative
Ocampo OO, Dela Paz DA, Talens SM, Roxas MFT, Regal HR, Monroy HJ, Go HL, Macalino JU, Ayuste EC, Valdez BEP, Cua LL, Simbulan MH and Herbosa TJ for the Committee on Trauma, Philippine College of Surgeons
Controversy has always beleaguered the care of the injured as far back as history can tell. Of these issues, none has been as controversial as the management of colon trauma. From its first description in the Book of Judges 1 until World War I, the repair of colon injuries has been fraught with abject failure. Due to poor outcome, Major General W.H. Ogilvie, consultant surgeon of the East African Command during the First World War, mandated obligatory colostomy for all colonic injuries. 2 The dictum was then adopted into civilian practice. For nearly 60 years, patients with colonic injuries were condemned to outright colostomy. Traditionally, 3 , 6 0 the criteria for obligatory colosto my were as follows: 1. Shock, preoperative BP <80/60 mmHg; 2. Hemorrhage, intraperitoneal blood loss > 1000ml; 3. Organs, > 2 intra-abdominal organ systems injured; 4. Contamination, significant peritoneal soilage by feces; 5. Time operation begun, >8 hours after injury; 6. Colon wound so destructive as to require resection; 7. Abdominal wall, major loss of substance/mesh placement. Developments in trauma care and experience in the Korean conflict and Vietnam War led some surgeons to challenge this long held concept. The landmark prospective study of Harlan Stone and Timothy Fabian comparing primary closure and exteriorization in 1979, laid the foundation for the modern day treatment of colon injuries. Subsequently, several studies confirmed the eff icacy and safety of primary repair in selected patients. The potential drawbacks of primary repair are the morbidity and mortality associated with suture line failure. If there is no difference in the morbidity and mortality between primary repair and co lostomy, primary repair would be preferred; however there is continued confusion as to when primary repair is appropriate. In an attempt to better define the appropriate roles of the surgical options (colostomy vs. primary repair) for penetrating colonic injuries, the Philippine College of Surgeons (PCS) through the Committee on Trauma decided to formulate these "Evidence-Based Clinical Practice Guidelines on the Management of Penetrating Colonic Injuries". It is envisioned that the application of this set of standards will be rewarded with decreased incidences of unnecessary colostomy and ill-advised primary repair for traumatic perforations of the colon. With proper use of the recommended management strategies, surgeons may be able to realize a higher rate of primary repair with its attendant lower morbidity and comparable mortality rates as compared to colostomy. The following were the clinical questions formulated by the Technical Working Group (TWG):
1. Can non-destructive penetrating colon injuries be repaired primarily? 2. What factors would make primary repair for non -destructive colon injuries a less likely option? 3. Can destructive penetrating colon injuries be repaired primarily? 4. What factors would make primary repair for destructive colon injuries a less likely option? The draft guidelines were presented to stakeholders during the Philippine College of Surgeons' Annual Convention held at the EDSA Shangri -la Hotel, Mandaluyong City on December 4, 2002. The invited participants inc luded practicing surgeons and surgical residents. The Evidence-Based Clinical Practice Guidelines in the Management of Penetrating Colonic Injuries were then submitted to the 2003 PCS Board of Regents for final approval in March, 2003.
Disclaimer of Liability The information contained in these guidelines reflects the current state of knowledge at the time of completion, October, 2002. The recommendations contained in these guidelines may not be appropriate for use in all circumstances. The decision to adopt any particular recommendation contained in these guidelines must be made by a treating physician in the light of all the facts and circumstances in each particular case and on the basis of the available resources. In view of the facts that there wi ll be future developments in scientific information and technology, it is anticipated that there will be a periodic review and updating of these guidelines. The validity of these guidelines is dated at 3 years.
Methods The Technical Working Group (TWG) was composed of : 1. Teodoro J. Herbosa, MD, FPCS - Chairman, PCS Committee on Trauma 2. Hermogenes R. Regal, MD, FPCS - Vice Chairman, PCS Committee on Trauma 3. Harry L. Go, MD, FPCS - Member, PCS Committee on Trauma 4. Joel U. Macalino, MD, FPCS - Member, PCS Committee on Trauma 5. Orlando O. Ocampo, MD, FPCS - Member, PCS Committee on Trauma 6. Eric SM. Talens, MD, FPCS - Vice President, Philippine Society for the Surgery of Trauma 7. Daniel A. Dela Paz, Jr. , MD, FPCS - Member, Philippine Society of General Surgeons 8. Hermogenes J. Monroy , MD, FPCS - Member, Philippine Society of Colon and Rectal Surgeons 9. Manuel Francisco T. Roxas, MD, FPCS - Member, PCS Committee on Research 10. Eduardo C. Ayuste, MD - Trauma Fellow, Philippine General Hospital 11. Benedict Edward P. Valdez, MD - Trauma Fellow, Philippine General Hospital
12. Leonardo L. Cua, MD, FPCS - Member, Board of Regent, PCS 13. Maximo H. Simbulan, MD, FPCS - Member Board of Regents, PCS A comprehensive computerized search was undertaken using Medline, Cochrane and Herdin libraries, the search included citations from 1975 to 2001 using the MeSH terms "colon injury/injuries", "colon trauma" and "colon repair". Textbook and relevant historical bibliographical articl es were reviewed and hand searched. From the search results, the TWG evaluated the abstract and selected relevant articles for full text retrieval. Of the 269 citations initially identified, the following groups of articles were eliminated from analysis: 1. Review articles 2. Letters to the editor 3. Animal studies 4. Articles dealing with technique and non -traumatic colon injuries Of the 120 articles that remained, 91 were chosen based on nominal group technique. Upon further evaluation, articles f rom institutions that were duplicative in nature were also excluded. A total of 60 articles evaluated and appraised by the TWG were included in the final analysis. The clinical evidence was then rated according to the assessment system of the Infectious Disease Society of America: Level I - Evidence from at least one properly designed randomized controlled trial or meta-analysis Level II Evidence from at least prospective cohort or case -control analytic studies, from multiple time -series studies, or from dramatic results in uncontrolled experiments. Level III- Evidence from opinions of respected authorities on the basis of clinical experience, descriptive studies, retrospective studies, or reports of expert committees. Members of the TWG prepared the evidence-based report based on the articles retrieved and appraised. The TWG together with the panel of experts reviewed the interim report on October 22, 2002 at the PCS Conference Room. The evidence and recommendations were scrutinized and the pa rticipants given the opportunity to express their opinions and views. The modified Delphi Technique, moderated by Dr. Earl Castillo (an epidemiologist), was then used to determine the degree of consensus regarding the recommendations. The strength of the r ecommendations was categorized according to the level of agreement of the panel of experts after a vote by the participants: Category A - Recommendations that were approved by consensus (75% of the expert panel) Category B Recommendations that were somewhat controversial and did not meet consensus. Category C - Recommendations that caused real disagreement among members of the panel.
The panel of experts included: 1. Bernardo M. Cuevas - Philippine Society of Colon and Rectal Surgeons 2. Beda R. Espineda - Philippine Society of Pediatric Surgeons 3. Celso M. Fidel - Philippine Society for the Surgery of Trauma 4. Dionisio T. Lopez - Philippine Association of Military Surgeons 5. Adriano V. Laudico - American College of Surgeons (Local Chapter ) 6. Narciso S. Navarro - Asian Surgical Association 7. Arsenio C. Pascual - International College of Surgeons 8. Isaac David E. Ampil II - PCS Committee on Surgical Research 9. Raymund Erese - PCS Committee on Surgical Research
Operational Definitions COLON - segment of bowel from the ileocecal valve to the sacral promontory PRIMARY REPAIR - Either of the following: (1) Debridement with simple closure of the perforation/s (2) Resection of a segment of bowel containing the perforation/s followed b y anastomosis COLOSTOMY - Any of the following: (1) Exteriorization of the injured colonic segment (2) Resection of the injured colonic segment with end colostomy (3) Primary repair of the injured colon with creation of a proximal stoma (ileostomy or colostomy) NON-DESTRUCTIVE COLON WOUNDS - colonic injuries that did not require resection DESTRUCTIVE COLON WOUNDS - any form of injury to the colon warranting resection CLINICALLY DETECTABLE PERITONITIS - inflammation of the peritoneum or serosal surfaces as evidenced by congestion and edema; presence of fibrinous, purulent, or fibrino-purulent; and/or frank abscess/es formation. STANDARD OF CARE - any intervention supported by at least level I evidence and approved by 75 per cent of the members of the panel
Summary of Guidelines 1. Can non-destructive penetrating colon injuries be repaired primarily? GUIDELINE 1. For non-destructive colonic injuries, the standard of care is primary repair.
LEVEL I EVIDENCE CATEGORY A RECOMMENDATION 2. What factors would make primary repair for non -destructive colon injuries a less likely option?
GUIDELINE 2. In non-destructive colonic injuries with clinically detectable peritonitis, colostomy is the primary option. LEVEL III EVIDENCE CATEGORY A RECOMMENDATION 3. Can destructive penetrating colon injuries be repaired primarily? GUIDELINE 3. Destructive colon injuries can be LEVEL II EVIDENCE CATEGORY A RECOMMENDATION 4. What factors would make primary repair for destructive colon injuries a less likely option? GUIDELINE 4. In destructive colonic injuries, colos -tomy is the primary option in the presence of any of the following: a. significant underlying medical illness b. clinically detectable peritonitis LEVEL III EVIDENCE CATEGORY A RECOMMENDATION a. hemodynamic instability b. significant associated intra-abdominal organ system injuries (>3) LEVEL III EVIDENCE CATEGORY B RECOMMENDATION repaired primarily.
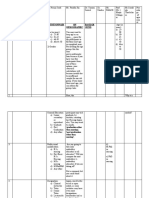
Guidelines 1. Can non-destructive penetrating colon injuries be repaired primarily? GUIDELINE 1. For non-destructive colonic injuries, the standard of care is primary repair. LEVEL I EVIDENCE CATEGORY A RECOMMENDATION There were 5 level I articles identified: 1 meta -analysis and 4 randomized controlled trials (RCT). Two RCTs were from the same institution. 5 , 6 The earlier study 5 was superseded by the latter, 6 which included 67 more patients. The former was considered duplicative and thus excluded.
The meta-analysis 4 showed a clear advantage of primary repair over colostomy with respect to post-operative complications. Odds ratio was 0.32 (0.13 -0.77). Two of the 3 RCT's were evaluated in this meta -analysis. 7 , 8 There were no suture line failures in the 71 patients who underwen t primary repair. The largest RCT 6 analyzed 176 patients, 81 of whom underwent colorrhaphy. There were no suture line failures. Two deaths occurred in this group, both non colon related. One hundred forty three (143) patients had colostomies, with a sin gle colon-related mortality. Morbidity rates for all RCT's are tabulated in Table 1. The results suggested that primary repair is at least as successful as colostomy, even when patients present with previously identified criteria for obligatory colostomy. There was one RCT 3 that the Technical Working Group classified as level II evidence. Forty eight percent (129 cases) of the study subjects were not randomized, and the concealment of allocation was clearly inadequate. 4 There was one suture line failure in 67 primary repairs. The morbidity rates for this study were 47.8 percent for primary repair and 56.9 percent for colostomy (p=0.361). There was one death in each group, both non -colon related. There were 41 level III articles, four of which were local publications. 9 - 1 2 Two articles 1 3 - 1 4 favored colostomy over primary repair with respect to postoperative complications. Three articles dealt exclusively with exteriorized repairs, 4 0 , 4 8 , 5 3 and were excluded from the analysis. The local publications report ed a leak rate of 0.8 per cent (3/372). There were 16 deaths (4.3%), all non -colon related. Sixty-eight patients had colostomies, with associated 10 per cent mortality. Overall morbidity rates were 17.2 and 19 percent for primary repair and colostomy, resp ectively. The rest of the articles 1 9 - 3 9 , 4 1 - 4 7 , 4 9 - 5 2 , 5 4 - 5 9 , 6 1 - 6 3 reported a total of 3191 cases of primary repair, with 35 suture line failures (1.09%). Seven deaths (0.2%) were attributable to these leaks. A total of 1619 colostomies were performed. Morbidity and mortality rates were 21.6 and 3.7 percent respectively. Some of the studies 3 4 , 4 9 reported increasing morbidities in cases where severe fecal contamination or peritonitis was noted. 2. What factors would make primary repair for non -destructive colon injuries a less likely option? GUIDELINE 2. In non-destructive colonic injuries with clinically detectable peritonitis, colostomy is the primary option. LEVEL III EVIDENCE CATEGORY A RECOMMENDATION Some of the retrospective studies 1 4 , 3 4 , 4 9 reported increasing leak rate in cases where peritonitis was present. However, there are no data comparing the leak rates in patients with to those without peritonitis. The definition of peritonitis also varied from study to study, making valid compariso ns difficult to achieve. 3. Can destructive penetrating colon injuries be repaired primarily? GUIDELINE 3. Destructive colon injuries can be repaired primarily.
LEVEL II EVIDENCE CATEGORY A RECOMMENDATION The level I articles 6 - 8 make a recommendation in favor of primary anastomosis for colon injuries requiring resection. However, in these studies, there were only 31 cases of resection anastomosis. There were no anastomotic leaks. Two patients died (7.1%) from non-colon related causes. The overall morbidity rates were 12.9 and 40.6 percent for resection-anastomosis and colostomy, respectively. A recent prospective study by Demetriades and cohorts 1 5 analyzed 297 patients, 197 of whom underwent primary anastomosis. There were 13 suture line fail ures (6.6%); none resulting in death. The overall incidence of colon related abdominal complications was 24 percent (primary repair, 22%; diversion, 27%; p=0.373). Morbidity increased in the presence of severe fecal contamination, transfusion of > 4 u blood within the first 24 hours and single agent prophylactic antibiotics. However, multivariate analysis, controlling for these confounding factors, showed no difference in outcome between primary anastomosis and colostomy (adjusted RR of 0.90: 95% CI 0.55-1.39; p = 0.64). The authors concluded that primary repair should be considered in such patients. 4. What factors would make primary repair for destructive colon injuries a less likely option? GUIDELINE 4. In destructive colonic injuries, option in the presence of any of the following: a. significant underlying medical illness b. clinically detectable peritonitis LEVEL III EVIDENCE CATEGORY A RECOMMENDATION c. hemodynamic instability d. significant associated intra-abdominal organ system injuries (>3) LEVEL III EVIDENCE CATEGORY B RECOMMENDATION In a prospective observational study, Cornwell and associates 1 6 analyzed 27 patients (25 primary repairs and 2 colostomies). There were 2 suture line failur es and both were fatal (8%). The authors surmised that there is still place for colostomy in high-risk patients with destructive colon injuries. In the level III studies 1 7 - 3 9 , 4 1 - 4 7 , 4 9 - 5 2 , 5 4 - 5 9 , 6 1 - 6 3 , 920 patients had resection anastomosis for destructive colon injuries. There were 34 anastomotic leaks (3.7%) with 4 colon-related mortalities (0.4%). The overall morbidity rates were 7.6 and 21.7 percent for primary anastomosis and colostomy, respectively. Most of the suture line failures were in those pa tients with associated significant intraabdominal injuries and/or disease processes. There are 2 level III studies that dealt exclusively with destructive colon injuries. Stewart 1 7 reported on 60 patients (43 managed by primary anastomosis and 17 by colostomy). Anastomotic leak rate was 14 percent (6/43). colo stomy is the primary
There was a 33 percent leak for patients who had medical illness and those who received more than 6 units of blood. Septic morbidity rates were 37 and 29 percent respectively. They concluded that primary repair should not be performed in these subsets of patients. The study of Murray et al 1 8 included 140 patients (112 primary anastomosis and 28 diversions). Anastomotic leak rate was 8 percent (9/112). Univariate analysis identified Pene trating Abdominal Trauma Index (PATI) >25 and hypotension in the emergency room to be associated with increased risk of anastomotic dehiscence. Septic morbidity rates were 29.5 and 29 percent respectively. The author suggested that in such cases, a diver sion procedure might be appropriate.
References
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. Holy Bible, Judges, Chapter 4, vers es 20 -25, King Jam es Version, Thomas Nels on (Candem), 1972. Im es PR. War surgery of th e abdomen. Surg Gynec ol Obstet 1945; 81:608. Stone HH and Fabian TC. Manag em ent of p erforating colon trauma: randomi zation bet ween primary closure and exteriori zation. Ann Surg 1979; 190: 430 -433. Ta lens E SM. Primary repair versus c olost om y in the managem ent of c olon injuries: A m eta -analysis. Philip J Surg Spec 1996; 51: 53-56. Gonza les RP, M erloti GJ, Holevar MR. Colost om y in penetrat ing colon injury: Is it nec es sary? J Trauma 1996; 41:271 -275. Gonza les RP, Falim erski ME, Holevar MR. Furth er evaluation of colostom y in pen etrating colon injury. Am Surg 2000; 66:342 -347. Chappius CW, Frey DJ, et al. Managem ent of penet rating colon injuries: A persp ective randomized trial. Ann Surg 1991; 213: 492 -497. Sasaki DS, Allaben RD, Galwa la R and Mittel VK. Prim ary repair of colon injuries: A pro spective randomized study. J Trauma 1995; 39:895 -901. Ng PC, Si oco S T, Joson RO a nd Gutierrez RR. The management of c olon and recta l trauma. Philip J Surg Sp ec 1981; 36:72 -80. Tan TN, Inao RS and de Vera R L. Colonic injuries: Managem ent in a r ural setting. Phili p J Surg Spec 1990; 45:80 -84. Padre R A, C risost omo AC and Silao J I. Factors affecting outcome of treatm ent of coloni c injuries: a review of 205 cases. Philip J Surg Sp ec 1993; 48:33 -38. Gi gantone R G. P rimary repair of traumat ic colon injury - a p rosp ective cas e s eries. Phi lip J Surg Sp ec 1997; 52:17 -19. Barwick J W and Schoffata ll R O. Routine exteriorization in the treatment of ci vilian colon injuries: A reappraisal. Am Surg 1978; 44:716 -722. Parks TG. Surgica l ma nagem ent of injuries of the large intes tine. Br J Surg 1981; 68: 725 -728. Dem etriades D, Murra y J A, C han L, et a l. Penetrating colon injuries requiring res ection diversion or primary anastomos es : An AAS T prospective, multicent er stu dy. J Trauma 20 01; 50:765 -775. Corn well FT, Velmahos GC, Berna JV, et a l. Th e fat e of colonic suture lines in high -risk trauma patients: a prospective analysis. J Am Coll Surg 1998; 187:58 -63. Stewa rt RM, Favian TC, et al. Is resection with primary anastomosi s following dest ructive colon wounds alwa ys safe? Am J Su rg 1994; 168:316 -319. Murray J A, Demitriades D, Cals on M, et al. Colonic res ection in trauma: colostom y vs. a nastomosis. J Trauma 1999; 46:250 -254. Dakucu A, Ozturik H, et a l. Colon injurie s in children. J Pediatr Surg 2000; 35:1799 -1804. Dente CJ, Tyburski J, et a l. Ostom y a risk factor for p ost -traumatic infection in penetrating colonic injuries: univariate and multivariate analysis. J Trauma 2000; 49:628 -634. Conrad JK, Ferry KM , et al. Changing managem ent trends in penetrating colon trauma. Dis Col R ec 2000; 43:466 -471. Murray J A. S evere colonic trauma requiring res ection : colostom y vs. anastomosis. J Trauma 1998; 44:424 -434. Berne J D, Belmaj os GC, et al. The high mo rbidity of colost om y closure aft er trauma: Further support for th e primary repair of c olon injuries. Surg 1998; 123:157 -164. Jacobson LE, Gom ez GA and Brondie TA. Primary repair of 58 consecutive penet rating injuries of the colon: Sh ould colost om y b e abandoned? Am Surg 1997; 63:170 -176. Durham RM, Prutt C, et a l. C ivilian colon trauma : factors t hat predict success b y prima ry repair. Dis Col R ec 1997; 40:685 -692. Velhamos GC, Sout er I, et a l. Primary repair for colonic gunshot wounds. Aust NZ J Surg 1996; 66:344 347. Moffoletto JP and Tate J S. Colon trauma: Primary repair evolving as d eep standard of care. J Natl Med Assoc 199; 88:574 -5786.
28. Miller BJ and Schache DJ. C olorectal injury: wh ere do we stand with repair? Au st NZ J Su rg 1996; 66:348 -352. 29. Bostick PJ, Hea rd JS, et al. Management of pen etrating colon injuries. J Nat Med As soc 1994; 86:378 382. 30. Sasaki LS, Mittal V and Alla ben RO. Primary repair of colon injuries: a retrospective analysis. Am Surg 1994; 60:522 -527. 31. Ivatury RR, Gaudino J, et a l. Definitive treatm ent of colon injuries: a prosp ective stud y. Am Surg 1993; 59:43 -49. 32. Schultz S Z, Magnant CM, et al. Id entifying the low -risk patient with penetrating colon ic injury for selective us e of primary re pair. Surg Gyn ecol Obstet 1993; 177:237 -242. 33. Morgado. Colon trauma -clinical staging in surgical decisi on -making. Dis Col Rec 1992; 35:986 -990. 34. Burch JM, Martin RR, et al. Evolution of the t reatment of the injured colon in the 1980's. Arch Surg 1991; 126:979 -983. 35. Levisi on M A, Thomas DD, et al. Managem ent of the injured c olon: evolving practice at an urban trauma center. J Trauma 1990; 30:247 -251. 36. George SM, Fabian TC, et al. P rimary repair of colon wounds. A p erspective tria l in non -selective patient. Ann Surg 1990; 212:118. 37. Nelken N and Lewis F. Th e Influenc e of injury s everit y on complication rate aft er prima ry c losure or colostom y for p enetrating colon trauma. Ann Surg 1989; 209:439 -447. 38. Fram e SV, Ridgewa y C A, et al. P e net rating injuries to the colon: analysis b y anatom ic region of injury. South Med J 1989; 82:1099 -1102. 39. George SM, Fabian TC and Mangiante EC. Colon trauma: further support for primary repair. Am J Surg 1988; 156:16 -20. 40. Nallathambi MN, Ivatury RR, et a l. Penetrating c olon injuries : ext eri ori zed repair vs. loop colostom y. Am Surg 1987; 203:209 -214. 41. Nallathambi M, Ivatury RR, et al. Penetrating ri ght colon trauma. The ever -diminishing role for colostom y. Am Surg 1987; 53:209 -214. 42. Burch JM, Brock JC, et al. Th e injured colon. Ann Surg 1986; 203:701 -711. 43. Shannon D. Primary repair of the colon: wh en is it a safe a lternative? Surg 98:851 -860. 44. Dem etriades D, Rabinowtiz B, et a l. Th e managem ent of colon injuries b y primary repa ir or colostom y. Br J Surg 1985; 72:881 -883. 45. Adkins RB and Waterh ouse G. Pen etrating colon trauma. J Trauma 1984; 24:491 -499. 46. Nallathambi MN, Ivatury RR, et a l. Aggressi ve definitive managem ent of pen etrating c olon injuries. 136 cases with 3.7 p ercent mortalit y. J Trauma 1984; 24:500 -505. 47. Hashmonai M, Torem S, et al. Primary repair of c olon injuries. Is r J Med Sci 1983; 19:116 -118. 48. Dang CV. Trauma of the c olon early drop back of exteriorized repair. Arch Surg 1982; 117:652 -656. 49. Ka rafi lian RG, Ghumann SS, et al. Pen etrating injuries to the colon. Am Surg 1982; 48:103 -108. 50. Thomps on JS and Moore EE. Factors affecting the outcome of ext eriori zed colon repairs. J Trauma 1982; 22:403 -406. 51. Thomps on JS, Moore EE and Moore JB. Compa rison of penetrating injuries of the right and left colon. Ann Surg 1981; 913:414 -428. 52. Slim MS, Makaroun M and Shamma AR. Primary repair in the managem ent of c olon injuries. Arch Surg 1981; 116:926 -929. 53. Lru M A, J ohnson AP, et al. E xteriori zed re pair in the management of colon injuries. Arc h Surg 1981; 116:926 -929. 54. Wi ener. Traumatic colon perforation: revi ew of 16 years experienc e. Am J Surg 1981; 142:717 -720. 55. Flint LM. The injured colon: relationships of management and complications. Ann Surg 1980; 193:619 623. 56. Thigpen JB, Santolices AA, et al. Current managem ent of trauma to the colon. S Afr Med J 1978; 53:95 -97. 57. Robbs JV. The a lt ernative t o colost om y for the injured colon. S. Afr M ed J 1978; 53:105 -107. 58. Ya w PB, Smith RN and Glover J L. Eight yea rs exp eri ence with civilian injuries of the colon. Surg Gynec ol Obstet 1977; 145:203 -205. 59. Robbs JV and Hegart y MM. The managem ent of c olon injuries. S Afr M ed J 1975; 49:1967 -1972. 60. Trauma Treatm ent Guidelines. PCS Sci entific Publication No. 10. 61. Cook A, Levin e B A, Rusing T. Traditional treatm ent of colon injuries: An effective m ethod. Arch Surg 1984; 119:591 -594. 62. Nwafo DC. S elective primary s uture of the battle injured colon: An experience of th e Ni geri an civil wa r. Br J Surg 1980; 67:195 -197. 63. Matolog NM, Wolfman E F. P rimary repair of c olonic injuries: A c linical eva luation. J Trauma 1977:544 546.
También podría gustarte
- Splenic Trauma WSES Classification and GuidelinesDocumento27 páginasSplenic Trauma WSES Classification and GuidelinespgmzAún no hay calificaciones
- The Clozapine Handbook - MeyerDocumento342 páginasThe Clozapine Handbook - MeyerMackie C100% (5)
- 089 Classification System For Complete EdentulismDocumento13 páginas089 Classification System For Complete EdentulismMihaela Gherghescu100% (1)
- Dentistry and Community IUST 010-011Documento72 páginasDentistry and Community IUST 010-011sharif100% (1)
- HEALTHDocumento28 páginasHEALTHKristine SaulerAún no hay calificaciones
- Documentation of Nutrition CareDocumento51 páginasDocumentation of Nutrition CareBrix ValdrizAún no hay calificaciones
- Compounding and DispensingDocumento9 páginasCompounding and DispensingElida Rizki MhAún no hay calificaciones
- A Guide To Field Notes For Qualitative Research: Context and ConversationDocumento9 páginasA Guide To Field Notes For Qualitative Research: Context and Conversationfrente amplio animalistaAún no hay calificaciones
- Quality Control in Endoscopy Unit: Safety Considerations For The PatientDocumento13 páginasQuality Control in Endoscopy Unit: Safety Considerations For The PatientPamela PampamAún no hay calificaciones
- JCC ECCO Endoscopy Consensus 11 2013 FINAL PDFDocumento37 páginasJCC ECCO Endoscopy Consensus 11 2013 FINAL PDFTikejdit BoukhamAún no hay calificaciones
- 01 - Jurnal Asli - Arman Caesar RamadhanDocumento21 páginas01 - Jurnal Asli - Arman Caesar Ramadhanarman caesar ramadhanAún no hay calificaciones
- American Society Ostomy SurgeryDocumento13 páginasAmerican Society Ostomy SurgeryvictorAún no hay calificaciones
- 190 Disc Repositioning Does It Really WorkDocumento23 páginas190 Disc Repositioning Does It Really WorkAngélica Valenzuela AndrighiAún no hay calificaciones
- The Tamil Nadu Dr. M.G.R Medical University: Dissertation Submitted ToDocumento129 páginasThe Tamil Nadu Dr. M.G.R Medical University: Dissertation Submitted ToAmmar AlnajjarAún no hay calificaciones
- Anatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFDocumento10 páginasAnatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFannisa ussalihahAún no hay calificaciones
- 2010 Mars Group Descriptive Epidemiology of The Multicenter ACL Revision Study (MARS) CohortDocumento8 páginas2010 Mars Group Descriptive Epidemiology of The Multicenter ACL Revision Study (MARS) CohortArmin ParavlićAún no hay calificaciones
- General OtolaryngologyDocumento1 páginaGeneral Otolaryngologyangela cañariAún no hay calificaciones
- Kassir 2021Documento10 páginasKassir 2021kwpang1Aún no hay calificaciones
- Per-Oral Endoscopic Myotomy (With Video) : Technology Status Evaluation ReportDocumento10 páginasPer-Oral Endoscopic Myotomy (With Video) : Technology Status Evaluation ReportMikael AngelooAún no hay calificaciones
- EAES SplinaDocumento28 páginasEAES SplinaachitulAún no hay calificaciones
- Dco 5 PDFDocumento10 páginasDco 5 PDFGauda GranthanaAún no hay calificaciones
- Bjs Znac302Documento12 páginasBjs Znac302Docteur FillaliAún no hay calificaciones
- WSES Splenic TraumaDocumento26 páginasWSES Splenic TraumaAndreas RendraAún no hay calificaciones
- Loop Vs DividedDocumento8 páginasLoop Vs DividedNatalindah Jokiem Woecandra T. D.Aún no hay calificaciones
- JCM 10 01853Documento16 páginasJCM 10 01853Katrina Mae FajardoAún no hay calificaciones
- Recuperación Postop ColorectalDocumento26 páginasRecuperación Postop ColorectalEspe LinAún no hay calificaciones
- A Prospective Comparativestudy of Open Versus Laparoscopic Appendectomy: A Single Unit StudyDocumento8 páginasA Prospective Comparativestudy of Open Versus Laparoscopic Appendectomy: A Single Unit StudyIJAR JOURNALAún no hay calificaciones
- 6037ASTR Astr 97 103Documento9 páginas6037ASTR Astr 97 103LuisNavarroHernandezAún no hay calificaciones
- A1504050119 PDFDocumento19 páginasA1504050119 PDFImam Hakim SuryonoAún no hay calificaciones
- Liver Trauma: WSES 2020 Guidelines: Review Open AccessDocumento15 páginasLiver Trauma: WSES 2020 Guidelines: Review Open AccessMayra HernandezAún no hay calificaciones
- JurnalDocumento35 páginasJurnalAndi MujtahidaAún no hay calificaciones
- Acceptance and Understanding of The Informed Consent Procedure Prior To Gastrointestinal Endoscopy by Patients: A Single-Center Experience in KoreaDocumento8 páginasAcceptance and Understanding of The Informed Consent Procedure Prior To Gastrointestinal Endoscopy by Patients: A Single-Center Experience in KoreaMariano SalvadorAún no hay calificaciones
- 0 Using The Modified Delphi Method To Establish ClinDocumento16 páginas0 Using The Modified Delphi Method To Establish ClinTheologos PardalidisAún no hay calificaciones
- GUIDELINE Inguinal Hernia Repair Toward Asian GuidelinesDocumento8 páginasGUIDELINE Inguinal Hernia Repair Toward Asian GuidelinesHendry Susanto100% (1)
- Acute Cholecystitis - PCP CPG 2003Documento37 páginasAcute Cholecystitis - PCP CPG 2003Teng IbanezAún no hay calificaciones
- EBM 2018 - Head and CancersDocumento136 páginasEBM 2018 - Head and CancersChandramohan SettyAún no hay calificaciones
- Laparoscopic Appendectomy PostoperativeDocumento6 páginasLaparoscopic Appendectomy PostoperativeDamal An NasherAún no hay calificaciones
- Hernia UmmaDocumento9 páginasHernia UmmaHeny KambuAún no hay calificaciones
- A Systematic Review of The Single-Stage Treatment of Chronic OsteomyelitisDocumento8 páginasA Systematic Review of The Single-Stage Treatment of Chronic Osteomyelitisrosa snakAún no hay calificaciones
- The Surgical Treatment of Esophageal Cancer Indications Comparative Analysis of Surgical TechniquesDocumento19 páginasThe Surgical Treatment of Esophageal Cancer Indications Comparative Analysis of Surgical Techniquesalinutza_childAún no hay calificaciones
- Incisional Hernia ThesisDocumento5 páginasIncisional Hernia Thesisgbwy79ja100% (1)
- Bun V34N3p223Documento6 páginasBun V34N3p223pingusAún no hay calificaciones
- International Journal of CardiologyDocumento9 páginasInternational Journal of CardiologyLiseahAún no hay calificaciones
- Japan Gastroenterological Endoscopy Society Guidelines For Colorectal Endoscopic Submucosal Dissection/endoscopic Mucosal ResectionDocumento21 páginasJapan Gastroenterological Endoscopy Society Guidelines For Colorectal Endoscopic Submucosal Dissection/endoscopic Mucosal ResectionJosseph EscobarAún no hay calificaciones
- Workshop Sessions: Abscess Drainage and ManagementDocumento1 páginaWorkshop Sessions: Abscess Drainage and ManagementDede MarizalAún no hay calificaciones
- Return To Preinjury Status After Routine Knee Arthroscopy in Military PopulationDocumento5 páginasReturn To Preinjury Status After Routine Knee Arthroscopy in Military PopulationLuis MiguelAún no hay calificaciones
- Laparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Documento5 páginasLaparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Juan Carlos SantamariaAún no hay calificaciones
- Utd 04524 Clinical - Article KunduzDocumento5 páginasUtd 04524 Clinical - Article Kunduzzenatihanen123Aún no hay calificaciones
- Surgical Versus Non-Surgical Treatment of Mandibular Condylar Fractures: A Meta-AnalysisDocumento22 páginasSurgical Versus Non-Surgical Treatment of Mandibular Condylar Fractures: A Meta-AnalysisHAún no hay calificaciones
- BCCBenchmarkingDocumento48 páginasBCCBenchmarkingوليد خالدAún no hay calificaciones
- Chest Wall Stabilization in Trauma Patients: Why, When, and How?Documento12 páginasChest Wall Stabilization in Trauma Patients: Why, When, and How?Ariane YudhiantiAún no hay calificaciones
- Clinical and Radiological Features of Incarcerated Hernia K7n3y0reDocumento5 páginasClinical and Radiological Features of Incarcerated Hernia K7n3y0reAndhika Reza AkbarAún no hay calificaciones
- Stapled Rectal Mucosectomy vs. Close HemorrhoidectomyDocumento9 páginasStapled Rectal Mucosectomy vs. Close HemorrhoidectomyNadllely Garcia ZapataAún no hay calificaciones
- WarshawDocumento11 páginasWarshawJuan RamirezAún no hay calificaciones
- Arthritis Rheumatology - 2021 - Chung - 2021 American College of Rheumatology Vasculitis Foundation Guideline For TheDocumento10 páginasArthritis Rheumatology - 2021 - Chung - 2021 American College of Rheumatology Vasculitis Foundation Guideline For TheDiana RamirezAún no hay calificaciones
- World Journal of Emergency Surgery: Preventable Trauma Deaths: From Panel Review To Population Based-StudiesDocumento7 páginasWorld Journal of Emergency Surgery: Preventable Trauma Deaths: From Panel Review To Population Based-StudiesRita RangelAún no hay calificaciones
- Decision Algỏithm and Surgical Strategies For Managing Trachecutaneous FistulaDocumento9 páginasDecision Algỏithm and Surgical Strategies For Managing Trachecutaneous Fistulahai1Aún no hay calificaciones
- Hemipelvectomia INCADocumento7 páginasHemipelvectomia INCAdrjccanciolopesAún no hay calificaciones
- Hand Transplantation Current Concepts and ManagemeDocumento10 páginasHand Transplantation Current Concepts and Managemeeliseoo8ortegaAún no hay calificaciones
- Management of Duodenal Trauma: Chinese Journal of Traumatology (English Edition) February 2011Documento5 páginasManagement of Duodenal Trauma: Chinese Journal of Traumatology (English Edition) February 2011dr muddssar sattarAún no hay calificaciones
- Clinical Spotlight Review - Intraoperative Cholangiography - A SAGES PublicationDocumento19 páginasClinical Spotlight Review - Intraoperative Cholangiography - A SAGES PublicationMu TelaAún no hay calificaciones
- 268 2011 Article 1088 PDFDocumento6 páginas268 2011 Article 1088 PDFIoel Tovar TrovaAún no hay calificaciones
- Case Studies of Postoperative Complications after Digestive SurgeryDe EverandCase Studies of Postoperative Complications after Digestive SurgeryAún no hay calificaciones
- Advanced Colonoscopy: Principles and Techniques Beyond Simple PolypectomyDe EverandAdvanced Colonoscopy: Principles and Techniques Beyond Simple PolypectomyToyooki SonodaAún no hay calificaciones
- The SAGES Manual of Flexible EndoscopyDe EverandThe SAGES Manual of Flexible EndoscopyPeter NauAún no hay calificaciones
- The SAGES Manual of Biliary SurgeryDe EverandThe SAGES Manual of Biliary SurgeryHoracio J. AsbunAún no hay calificaciones
- STD 12 Science Group B Ready Recknor VDocumento36 páginasSTD 12 Science Group B Ready Recknor Vfree accag100% (2)
- Format Pencatatan Hasil RSUD SR GABUNGDocumento90 páginasFormat Pencatatan Hasil RSUD SR GABUNGLuluk SetiawanAún no hay calificaciones
- Physical Education and Health 12Documento2 páginasPhysical Education and Health 12Jenia Alexis CapaAún no hay calificaciones
- LA Low Cost Dog NeuteringDocumento2 páginasLA Low Cost Dog Neuteringtonys71Aún no hay calificaciones
- Experts Validation TableDocumento20 páginasExperts Validation TableDeepti KukretiAún no hay calificaciones
- Assesment of Knowledge of Analgesic Drugs in Pregnant WomenDocumento6 páginasAssesment of Knowledge of Analgesic Drugs in Pregnant WomenMahrukh AmeerAún no hay calificaciones
- Data India 250 BDocumento14 páginasData India 250 BmuruganjdAún no hay calificaciones
- Proposal DraftDocumento15 páginasProposal DraftDagimAún no hay calificaciones
- Laterally Closed Tunnel Sculean Allen IJPRD 2018 PDFDocumento11 páginasLaterally Closed Tunnel Sculean Allen IJPRD 2018 PDFVladAlexandruSerseaAún no hay calificaciones
- Research ArticleDocumento4 páginasResearch ArticleAnu SharmaAún no hay calificaciones
- Kajang ScriptDocumento6 páginasKajang ScriptK EV INAún no hay calificaciones
- Ella - (Effective Reporting and Record-Keeping in Health and Social Care Services)Documento8 páginasElla - (Effective Reporting and Record-Keeping in Health and Social Care Services)Rajesh KumarAún no hay calificaciones
- M.Ch. CVSDocumento43 páginasM.Ch. CVSRithikaAún no hay calificaciones
- Communication For Managers: Group Assignment No. 1Documento25 páginasCommunication For Managers: Group Assignment No. 1Namit BaserAún no hay calificaciones
- Kep KritisDocumento193 páginasKep Kritisari cahyaAún no hay calificaciones
- List of Specialist Accredited Hospitals (Metro Manila)Documento20 páginasList of Specialist Accredited Hospitals (Metro Manila)Jimbo OctagonAún no hay calificaciones
- "Optimization of Instrumental Workflow in CSSD" at Hospital SectorDocumento6 páginas"Optimization of Instrumental Workflow in CSSD" at Hospital SectorIndra PratamaAún no hay calificaciones
- Advanced Process MappingDocumento35 páginasAdvanced Process MappingJustformedia JustformediaAún no hay calificaciones
- Hope 2 ParqDocumento1 páginaHope 2 ParqJohn Michael PanganAún no hay calificaciones
- I Sometimes Worry About My Short Attention SpanDocumento1 páginaI Sometimes Worry About My Short Attention SpanAmmer Yaser MehetanAún no hay calificaciones
- Consimtamantul InformatDocumento6 páginasConsimtamantul Informatr_lilianaAún no hay calificaciones
- Approved Internship Sites As at 31st January 2024Documento2 páginasApproved Internship Sites As at 31st January 2024simwingamaxwellAún no hay calificaciones
- Lactao Morella Kristina C. Journal Surgery WardDocumento1 páginaLactao Morella Kristina C. Journal Surgery WardKeyceeleen Guevarra LimAún no hay calificaciones