Documentos de Académico
Documentos de Profesional
Documentos de Cultura
An Overview of Dry Socket and Its Management: S. Preetha
Cargado por
Rossye MpfDescripción original:
Título original
Derechos de autor
Formatos disponibles
Compartir este documento
Compartir o incrustar documentos
¿Le pareció útil este documento?
¿Este contenido es inapropiado?
Denunciar este documentoCopyright:
Formatos disponibles
An Overview of Dry Socket and Its Management: S. Preetha
Cargado por
Rossye MpfCopyright:
Formatos disponibles
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861. Volume 13, Issue 5 Ver. II. (May. 2014), PP 32-35
www.iosrjournals.org
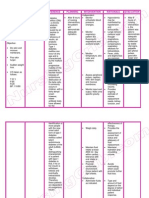
An Overview of Dry Socket and Its Management
S. Preetha
Saveetha Dental College Ponamallee, Chennai
Abstract: Dry socket is one of the common complication after the removal of third molars. It occurs due to
disruption of the clot within the socket. This article gives a brief overview about the clinical features,
etiopathogenesis and the management of dry socket.
Key words: alveolar osteitis , fibrinolysis , management
I.
Introduction
A dry socket also referred to as alveolar osteitis is a post operative complication that interferes with the
healing process that takes place after a tooth extraction. Blum (2002) defined alveolar osteitis as post operative
pain inside and around the extraction site , which increases in severity at any time between the first and third
day after the extraction ,accompanied by a partial or total disintegrated blood clot within the alveolar socket
with or without halitosis.1
Dry socket was first described by Crawford in 1896. 2 The name dry socket is used because the socket
has a dry appearance after the blood clot is lost and debris washed away. The other terms used are alveolar
osteitis , alveolitis , localized osteitis , alveolitis sicca dolorosa , localized alveolar osteitis , fibrinolytic alveolitis
, septic socket , necrotic socket , alveolagia.3 It occurs when the tooth socket loses the blood clot that forms after
the tooth is extracted and the bone inside the socket is exposed. It occurs in 0.5-5% of routine dental extractions
and 25-30% in extraction of impacted mandibular third molars.4
II.
Clinical Features
Clinically , an empty socket which lacks a blood clot and exposed bone are seen. The socket may be
filled with food debris and saliva mixture. 4 Pain starts 24-72 hours after extraction. It varies in frequency and
intensity and radiates to the ear and neck.5 Headache , insomnia and dizziness may be present.6 It is not
characterized by redness , swelling , fever or pus formation but oedema of the surrounding gingiva and regional
lymphadenitis is present. There is marked halitosis and foul taste. 7,8
Histological features of dry socket is comprised of remenants of the blood clot and a massive
inflammatory response characterized by neutrophils and lymphocyte which may extend into the surrounding
alveolus.9
III.
Etiopathogenesis
Several theories have been proposed on the etiology of dry socket . They are trauma during extraction ,
bacterial infection and biochemical agents.10 Fibrinolysis is a normal physiological process that removes fibrin
deposits by enzymatic digestion of the fibrin meshwork into smaller soluble fragments. Local increase in
fibrinolysis occur in response to bleeding.11
Birn in 1973 showed that there is increased fibrinolytic activity in dry sockets and activation of
plasminogen to plasmin in the presence of tissue activators. 9 He also proposed that the increase in fibrinolysis
decreased the chance of dissolution of the blood clot before the second day after surgery , because the clot
contains antiplasmin , which must be neutralized before clot dissolution can occur. 12
A fibrin clot is formed by thrombin and fibrinogen in a normal post extraction socket. Over this , the
epithelium migrates. New blood vessels grow into the clot during granulation tissue formation and this clot
degrades through the activity of fibroblast and fibrinolysis through the plasmin before the start of
osteoproliferation.13 Birn discovered that the plasmin like activity in dry sockets was not present at normal
extraction sites.14 Kinases are liberated during inflammation through direct or indirect activation of plasminogen
in the blood. These kinases cause lysis and destruction of the blood clot. Tissue or plasma pro-activators and
activators convert the plasminogen to fibrin , resulting in the dissolution of the clot by disintegration of fibrin. 15
This plasminogen pathway activation , can be direct(physiologic) or indirect(non physiologic) activators. Direct
activators are released to the alveolar bone cells after trauma. Indirect activators are released by bacteria. 16,17
Direct extrinsic activators are tissue plasminogen activators and endothelial plasminogen activators. Direct
intrinsic activators include the components of plasma such as factor XII , urokinase. Birn showed that the kinin
in concentration as low as 1mg/ml produce intense pain.18
www.iosrjournals.org
32 | Page
An Overview of Dry Socket and Its Management
IV.
Predisposing Factors
Extraction Site
Dry sockets occur more frequently in the mandible than the maxilla due to thick cortical bone resulting
in poor perforation of blood supply the mandible. It occurs more commonly in the extraction of the third
molars.19
Gender
It occurs more frequently in females than males due to possible hormonal cause. Sweet and
Butler(1938) reported that the incidence of dry socket in females is 4.1% compared to males.20
Trauma
Difficult extractions occur in older and dense bone which may have a decreased vascularity. Birn
proposed that trauma from extraction and aggressive curettage cause the inflammation of the alveolar osseous
medulla which leads to the release of cell mediators. This causes fibrinolytic activity. 9
Smoking
Smoking reduce the neutrophil chemotaxis and phagocytosis thus impairing the production of
immunoglobulin.21 Nicotine the active drug in tobacco is absorbed though the oral mucosa. This drug increases
the platelet aggregation thereby increasing the risk of microvascular thrombosis and peripheral ischemia.
Proliferation of fibroblast and macrophages is also inhibited. 22
The incidence of dry socket was significantly higher in smokers (12%) than in non-smokers (4%) , but,
there is a strong association between the amount of smoking and the incidence of dry socket. 23
Vasoconstrictors
Vasoconstrictors in the local anesthetics used for extraction may also contribute to the formation of dry
socket. Vasocinstrictors cause temporary local ischemia which increase the risk of developing alveolar
osteitis.9,24
Microorganisms
Bacteria may also play a contributing factor in the etiology of dry socket. Delayed healing may occur
due to the presence of microorganisms like Enterococcus , Streptococcus viridans , Bacillus coryneform ,
Proteus vulgaris , Pseudomonas aeruginosa , Citrobacter freundii , Escheria coli.
Nisan et al (1983) proposed that the anaerobic bacteria Treponema denticola showed plasminogen like
fibrinolytic activity.3
Oral Contraceptives
Lily observed that the dry socket occurred three times more frequently in females on oral
contraceptives than in those who were not taking them. Oral contraceptives elevate plasma fibrinolytic activity
which affects the stability of the clot after extraction. They elevate the factors II, VII,VIII,X and plasminogen
thereby increasing the lysis of blood clot.25
Radiotherapy
Radiotherapy to the head and neck results in a decreased blood supply to the mandible .26
V.
Prevention
Chlorhexidine
Chlorhexidine(CHX) is a bisguanide antiseptic which when used as a preoperative irrigant and
mouthwash , reduce the quantity of oral microbiota.
www.iosrjournals.org
33 | Page
An Overview of Dry Socket and Its Management
Field et al(1987) observed that there was a decreased incidence of dry socket after irrigation of the
gingival crevice and two minute mouth rinse with 0.2% CHX digluconate in comparison with no irrigation or
irrigation with saline. 13
Study was conducted in a private practice setting to determine the effect of a 0.12% chlorhexidine gluconate
rinse (Peridex, Proctor and Gamble, Cincinnati, Ohio) on the incidence of dry socket after removal of impacted
mandibular third molars. Over a 3-year period, 371 patients (total of 654 impacted mandibular third molars)
received either no treatment (group 1), 2 weeks of twice daily Peridex rinse postsurgery (group 2), or one rinse
presurgery (group 3). The group that used Peridex twice daily for 2 weeks after surgery (group 2) showed a
significant reduction (56%) in the incidence of dry socket when compared with either the group that did not
rinse (group 1) or the group that rinsed only once just before surgery (group 3). 27
Antibiotics
Systemic and topical antibiotics influence the incidence of dry socket. 28 Systemic antibiotics like
Penicillin , Clindamycin , Erythromycin and Metronidazole are effective in prevention of dry socket. Use of
topical tetracyclines has shown side effects along with foreign body reactions. 17
Antifibrinolytics
Antifibrinolytics like traxanemic acid interfere with the formation of the fibrinolytic enzyme plasmin
from its precursor plasminogen by plasminogen activators. 17
Antimicrobial Photo Dynamic Therapy(Apdt)
Lower incidence of dry socket after antimicrobial photodynamic therapy seems to be a new and
promising possibility for the prevention of alveolar osetitis.
In a study , the group with aPDT alveolar ostitis occurred at one extraction site and in the control group
without aPDT in 13 cases, the subjective pain assessment on the day after tooth removal was scored with
11.2+/-9.8 in the aPDT-group and with 19.0+/-12.2 in the control group. One week after extraction the pain
sensation in the aPDT group was scored with 2.4+/-9.2 and in the control group with 13.1+/-25.2. The
difference was significantly lower with p=0.000 for the 1st and 8th post-surgical days in the aPDTgroup.29
Low Level Laser Therapy(Lllt)
LLLT increases the speed of wound healing and reduces inflammation when compared to Alvogyl and
Salilept. It is used after the irrigation of socket as a continuous mode diode laser irradiation (808 nm, 100 mW,
60 seconds, 7.645/cm)30
VI.
Management
Management of dry socket can be by irrigation , surgical intervention and placement of medicated dresssing.
Irrigation
Irrigation removes the debris , sequestra and bacteria from the denuded bone in the dry socket. 31 The
use of heated saline solution , powdered sodium perborate , gauze with iodoform , the prescription of codeine
and subsequent irrigation with a concentrated solution of sodium perborated has been proposed in 1929. 32 Home
instructions for maintenance of oral hygiene and gentle warm saline rinses help in the healing of the socket. 8
Medicated Dressing
Placement of medicated dressing is suggested as a combination with surgical intervention due to the
occurrence of local complications.33 Turner proposed that packing of the socket could delay wound healing and
increases the chance of infection. Fazakerley and Field suggested the removal of sutures and irrigation with
warm saline under local anesthesia before the applicationof a medicated dressing containing zinc oxide and
eugenol mixed into a semisolid consistency applied to an iodoform ribbon gauze. Every 2-3 days , the pack
must be changed and removed after the pain subsides.13 Use of pertoleum based carriers is not recommeded due
to myospherulosis. Some of the medicated dressings used are antibacterials, topical anesthetics and obtundants,
or combinations of all three, e.g., zinc oxide and eugenol impregnated cotton pellets, alvogyl (eugenol, iodoform
and butamen), dentalone, bismuth subnitrate and iodoform paste (BIPP) on ribbon gauze and metronidazole and
lidocaine ointment.34
Analgesics
The choice of analgesics can range from a short course of non steroidal antiinflammatory drug to
narcotic based like codeine.
www.iosrjournals.org
34 | Page
An Overview of Dry Socket and Its Management
Surgical Intervention
Curretage can be used as a method of treatment for dry socket. However it is not recommended due to
the induction of more pain. Curretage involves administration of anesthesia , surgical debridement of socket and
primary closure by advancement flap.23 Turner stated that curretage and removal of granulation tissue resulted
in fewer visits than zinc oxide eugenol or iodoform gauze with eugenol technique.
VII.
Conclusion
The occurrence of dry socket is unavoidable. It canbe prevented by copious use of irrigation, antibiotics
and maintenance of oral hygiene. Although there is no specific treatment for dry socket eugenol dressings and
curretage reduce the incidence of it.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
[11].
[12].
[13].
[14].
[15].
[16].
[17].
[18].
[19].
[20].
[21].
[22].
[23].
[24].
[25].
[26].
[27].
[28].
[29].
[30].
[31].
[32].
[33].
[34].
[35].
Blum IR. Contemporary review on dry socket(alveolar osteitis):a clinical appraisal of standardization , aetiopathogenesis and
management :a critical review. International Journal of Oral and Maxillofacial Surgery 2002;3(3):309-317 [Pub Med]
Crawford JY.Dry socket . Dental Cosmos. 1896;38:929-931
Cadoso CL, Rodrigues MT , Ferreira JO , Garlet GP , de Carvalho PS.Clinical concepts of dry socket .J Oral Maxillofac Surg
2010;68:1922-1932
Bowe DC , Rogers S , Stassen LF. The management of dry scocket/alveolar osteitis .J Ir Dent Assoc 2011;57:305-310
Swanson AE:A double blind study on the effectiveness of tetracycline in reducing the incidence of fibrinolytic alveolitis. J Oral
Maxillfac Surg 47:165,1989
Sasaki T.Okamoto T:Topical treatment of infections of alveolar socket infections following dental extractions. Rev.Bras Odontol
25:82,1968
Awang MN.The aetiology of dry socket :a review .Int Dent J 1989;39:236-40
Fazakerley M.Field EA.Dry socket:A painful post extraction complication(a review).Dent Update 1991;18:31-4
Birn H. Etiology and pathogenesis in fibrinolytic alveolitis (dry socket). Int J Oral Surg 1973;2:211-63
Butler DP, Sweet JB.Effect of lavage on the incidence of localized osteitis in mandibular third molar extraction sites.Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 1977;44:14-20
Catellini JE.Review of factors contributing to dry socket through enhanced fibrinolysis . J Oral Surg. 1979;37:42-46
Birn H.Bacteria and fibrinolytic activity in dry socket Acta Odontol Sand 1970;28:773-83
Houston JP , McCollum J , Pietz D , Schneck D . Alveola osteitis :a review of its etiology , prevention and treatment modalities .
Gen Dent 2002;50:457-63
Birn H. Fibrinolytic activity of normal alveolar bone. Acta Odontol Scand 1971;29:141-53
Birn H.Fibrinolytic activity of normal alveolar bone. Acta Odontol Scand 1972;23-32
Daly B , Sharif MO , Newton T , Jones K , Worthington HV. Local interventions for the management of alveolar osteitis (dry
socket). The cochrane Library 2012;12:1-30
Kolokythas A , Olech E , Miloro M . Alveolar osteitis : a comprehensive review of concepts and controversies. Int J Dent 2010;1-10
Birn H. Kinins and pain in dry socket . Int J Oral Surg . 1972;1:32-42
Muhammad AS. Pathogenesis and management of dry socket(alveolar osteitis). Pakistan Oral and Dental Journal Vol 30 ,
No.2(December 2010)
Sweet DB , Butler DP. Predisposing and operative factors:effect on the incidence of localized osteitis in mandibular third molar
surgery. Oral Surg Oral Med Pathol 1978;46(2):206-213
Noroozi AR , Philbert RF. Modern concepts in understanding the management of the dry socket syndrome:comprehensive review
of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:30-35
Silverstein P. smoking and wound healing .AmJ Med 93:22,1992
Mohammed H Abu Younis and Ra'ed O Abu Hantash. Dry Socket: Frequency, Clinical Picture, and Risk Factors in a Palestinian
Dental Teaching Center.Open Dent J. 2011; 5: 712.
Fridrich , K.L , Olson , R.A. Alveolar osteitis following surgical removal of mandibular third molars. Anesth Prog 1990;(1)32-41
Lily GE , Osbon DB , Rael Em , Samuels HS , Jones JC . Alveolar osteitis associated with mandibular third molar extractions.
JADA 1974;88:802-6
Soames JV; Southam JC (1999). Oral pathology (3. ed., [Nachdr.] ed.). Oxford [u.a.]: Oxford Univ. Press. pp. 296298.
Bonine FL .Effect of chlorhexidine rinse on the incidence of dry socket in impacted mandibular third molar extraction sites Oral
SurOralMed Oral Pathol Oral Radio Endol.. 1995 Feb;79(2):154-7; discussion 157-8.
Torres-Lagares D. Serera-Figallo MA , Romero-Ruiz MM , Infante-Cossio P , Garcia M , Gutierez-Perez JL. Update on dry socket :
a review of the literature. Med Oral Patol Oral Cir Bucal 2005;10:81-85
NeugebauerJ, Jozsa M, Kbler A. Antimicrobial photodynamic therapy for prevention of alveolar ostitis and post-extraction pain.
2004 Nov;8(6):350-5. Epub 2004 Sep 29.
Kaya GS , Yapici G , Sarvas Z , Gungormus M . Comparison of alvogyl , Salicept patch and low level laser therapy in the
management of alveolar osteitis. J Oral Maxillofac Surg 2011;69:1571-1577
Betts NJ , Makowski G , Shen YH , Hersh EV. Evaluation of topical viscous 2% lidocaine jelly as an adjunct during the
management of alveolar osteitis. J Oral Maxillofac Surg 1995;53:1140-4
Schroff J , Bartels HA:Painful sockets after extractions. A preliminary report on the investigation of heir etiology , prevention and
treatment (abstract). Dent Res J 9:81,1929
Ogini FO , Fatusi OA , Alagbe AO. A clinical evaluation of dy socket in a Nigerian population. Oral Maxillofac Surg. 2003.61:87176
Daly, B; Sharif, MO; Newton, T; Jones, K; Worthington, HV (Dec 12, 2012). "Local interventions for the management of alveolar
osteitis (dry socket)
Turner PS. A clinical study of dry socket. Int J Oral Surg 1982;11:226-31
www.iosrjournals.org
35 | Page
También podría gustarte
- Pa Tho Genesis and Management of Dry SocketDocumento4 páginasPa Tho Genesis and Management of Dry SocketNina AbdulAún no hay calificaciones
- Dry SocketDocumento32 páginasDry Socketwaqas iqbalAún no hay calificaciones
- Oral Surgery Final2Documento8 páginasOral Surgery Final2mahmoodAún no hay calificaciones
- Prevention of Alveolar Osteitis: A Case Report and Review of LiteratureDocumento5 páginasPrevention of Alveolar Osteitis: A Case Report and Review of Literaturechandra auliaAún no hay calificaciones
- Dry Sockets - A Systemic ReviewDocumento10 páginasDry Sockets - A Systemic ReviewBrachmedio B. S. EAún no hay calificaciones
- Jurnal 2Documento6 páginasJurnal 2yesikaichaaAún no hay calificaciones
- 247 PDFDocumento5 páginas247 PDFRossye MpfAún no hay calificaciones
- A Case Report of Sodium Hypochlorite AccidentDocumento4 páginasA Case Report of Sodium Hypochlorite AccidentDaniela RochaAún no hay calificaciones
- Dis IcDocumento11 páginasDis IcyeandunAún no hay calificaciones
- Endophthalmitis: Please ShareDocumento9 páginasEndophthalmitis: Please ShareAnnisaAún no hay calificaciones
- ESCRS EndophthalmitisDocumento52 páginasESCRS EndophthalmitisKaveh Vahdani100% (2)
- Dry SocketDocumento20 páginasDry SocketHosuru SwethaAún no hay calificaciones
- Management of Post-Operative Endophthalmitis: A ReviewDocumento8 páginasManagement of Post-Operative Endophthalmitis: A ReviewIJAR JOURNALAún no hay calificaciones
- Oral Management of Idiopathic Thrombocytopenic Purpura Patient: Case ReportDocumento5 páginasOral Management of Idiopathic Thrombocytopenic Purpura Patient: Case ReportNauroh NaurohAún no hay calificaciones
- CD 4Documento8 páginasCD 4Amira AlmutairiAún no hay calificaciones
- Pterygium Excision and Conjunctival AutograftDocumento13 páginasPterygium Excision and Conjunctival Autograftgrace liwantoAún no hay calificaciones
- Accidente in Cazul Utilizarii Hipocloritului de SodiuDocumento4 páginasAccidente in Cazul Utilizarii Hipocloritului de SodiuTraian IlieAún no hay calificaciones
- JIAOMR5Documento5 páginasJIAOMR5Sweetz Viena ParamitaAún no hay calificaciones
- Infectious Endophthalmitis After: CataractDocumento6 páginasInfectious Endophthalmitis After: CataractSurendar KesavanAún no hay calificaciones
- Dry Socket (Alveolar Osteitis) : Incidence, Pathogenesis, Prevention and ManagementDocumento4 páginasDry Socket (Alveolar Osteitis) : Incidence, Pathogenesis, Prevention and ManagementPipin HeryantoAún no hay calificaciones
- Hemostab, Blknktic AgentsDocumento7 páginasHemostab, Blknktic AgentsashajangamAún no hay calificaciones
- Cyclosporin Induced Gingival Overgrowtrh-A Case Report K. Malathi, Muthu Kumaraswamy, Pushpinder SandhuDocumento11 páginasCyclosporin Induced Gingival Overgrowtrh-A Case Report K. Malathi, Muthu Kumaraswamy, Pushpinder SandhudellalalaAún no hay calificaciones
- Abcess PeritonsillarDocumento21 páginasAbcess PeritonsillarribeetleAún no hay calificaciones
- Practical Trends in Anesthesia and Intensive Care 2018De EverandPractical Trends in Anesthesia and Intensive Care 2018Aún no hay calificaciones
- Ultrasound-Guided Botulinum Toxin-A Injections Sialorrhea - BARBERO 2016Documento7 páginasUltrasound-Guided Botulinum Toxin-A Injections Sialorrhea - BARBERO 2016Adriana BragaAún no hay calificaciones
- Goo Jurnal MukokelDocumento4 páginasGoo Jurnal MukokelRhea Zarna IrsataniAún no hay calificaciones
- Decontamination of Titanium Implant Surface and Re-Osseointegration To Treat Peri-Implantitis: A Literature ReviewDocumento12 páginasDecontamination of Titanium Implant Surface and Re-Osseointegration To Treat Peri-Implantitis: A Literature ReviewAlejandra Del PilarAún no hay calificaciones
- Endophthalmitis - Prophylaxis - For - Cataract - Surgery PDFDocumento6 páginasEndophthalmitis - Prophylaxis - For - Cataract - Surgery PDFDwi PascawitasariAún no hay calificaciones
- Recent Advancements in Management of Alveolar Osteitis (Dry Socket)Documento5 páginasRecent Advancements in Management of Alveolar Osteitis (Dry Socket)International Journal of Innovative Science and Research TechnologyAún no hay calificaciones
- Mukokel OralDocumento4 páginasMukokel OralIlma Kurnia SariAún no hay calificaciones
- Rhinology 2002 p185Documento4 páginasRhinology 2002 p185Rettha SigiroAún no hay calificaciones
- Proptosis UnilateralDocumento5 páginasProptosis UnilateralCarlos NiveloAún no hay calificaciones
- Cap 3Documento24 páginasCap 3Elena DimitriuAún no hay calificaciones
- Alveolar OsteitisDocumento42 páginasAlveolar OsteitisBastosTemitayoStephen100% (2)
- Complications During Root Canal Irrigation - Literature Review and Case ReportsDocumento8 páginasComplications During Root Canal Irrigation - Literature Review and Case ReportsGavi GazAún no hay calificaciones
- Vitrectomy in Endophthalmitis: Kapil Bhatia, Avinash Pathengay and Manav KheraDocumento17 páginasVitrectomy in Endophthalmitis: Kapil Bhatia, Avinash Pathengay and Manav KheraGrady ChristianAún no hay calificaciones
- Systemic Review of Dry Socked Aetiology Treatment and PreventionDocumento4 páginasSystemic Review of Dry Socked Aetiology Treatment and PreventionAnnisa MardhatillahAún no hay calificaciones
- Root Resorption Diagnosis, Classification and Treatment Choices Based On Stimulation FactorsDocumento8 páginasRoot Resorption Diagnosis, Classification and Treatment Choices Based On Stimulation FactorsAhmad AssariAún no hay calificaciones
- Antibiotic Medicaments ReviewDocumento10 páginasAntibiotic Medicaments ReviewGeorge ChackoAún no hay calificaciones
- Eksternal HemorrhoidDocumento13 páginasEksternal HemorrhoidJanelle MooreAún no hay calificaciones
- Efficacy of Intra-Alveolar Chlorhexidine Gel in Reducing Frequency of Alveolar Osteitis in Mandibular Third Molar SurgeryDocumento4 páginasEfficacy of Intra-Alveolar Chlorhexidine Gel in Reducing Frequency of Alveolar Osteitis in Mandibular Third Molar SurgeryCahyo AdyAún no hay calificaciones
- Root Bio Modification PerioDocumento37 páginasRoot Bio Modification PerioFourthMolar.com100% (1)
- Epithelial DowngrowthDocumento5 páginasEpithelial Downgrowthaghnia jolandaAún no hay calificaciones
- Peri Implantitisetiologydiagnosisandmanagement PDFDocumento49 páginasPeri Implantitisetiologydiagnosisandmanagement PDFRobins DhakalAún no hay calificaciones
- Dry SocketDocumento15 páginasDry Socketbadar_aq100% (1)
- Steroid KeratitisDocumento8 páginasSteroid KeratitisNanda Wiguna TyndiansyahAún no hay calificaciones
- Intl Journal of Cancer - 2014 - Landeck - Handling Chemotherapy Drugs Do Medical Gloves Really ProtectDocumento6 páginasIntl Journal of Cancer - 2014 - Landeck - Handling Chemotherapy Drugs Do Medical Gloves Really ProtectPhạm Thu HuyềnAún no hay calificaciones
- Steroids and Antiobiotics in TonsillectomyDocumento9 páginasSteroids and Antiobiotics in TonsillectomyjulianasanjayaAún no hay calificaciones
- Dry Socket (Alveolar Osteitis) Is A Postoperative Pain Around Tooth's Socket That CanDocumento6 páginasDry Socket (Alveolar Osteitis) Is A Postoperative Pain Around Tooth's Socket That CanDindaAún no hay calificaciones
- Untitled 3Documento10 páginasUntitled 3Satya AsatyaAún no hay calificaciones
- PilonidalDocumento12 páginasPilonidalLuis RuizAún no hay calificaciones
- Mohamed Omaia, Maged Negm, Yousra Nashaat, Nehal Nabil, Amal OthmanDocumento11 páginasMohamed Omaia, Maged Negm, Yousra Nashaat, Nehal Nabil, Amal OthmancarlosAún no hay calificaciones
- Iatrogenic Factors and Oral HealthDocumento7 páginasIatrogenic Factors and Oral HealthVineet ArunAún no hay calificaciones
- Tugas BM 1 Panji Dry SocketDocumento8 páginasTugas BM 1 Panji Dry SocketPanji HrAún no hay calificaciones
- Current Approach of Management of Post Operative EndoftalmitisDocumento10 páginasCurrent Approach of Management of Post Operative EndoftalmitisyyyyAún no hay calificaciones
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentDe EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentAún no hay calificaciones
- Complications in UveitisDe EverandComplications in UveitisFrancesco PichiAún no hay calificaciones
- Glaucoma A Symposium Presented at a Meeting of the Chicago Ophthalmological Society, November 17, 1913De EverandGlaucoma A Symposium Presented at a Meeting of the Chicago Ophthalmological Society, November 17, 1913Aún no hay calificaciones
- Practical Issues in Anesthesia and Intensive Care 2013De EverandPractical Issues in Anesthesia and Intensive Care 2013Aún no hay calificaciones
- Analisis Pemakaian Jasa Pemasangan Gigi Tiruan Sebagian Lepasan Akrilik Pada Dokter Gigi Dan Tukang Gigi Di Desa Peuniti Banda AcehDocumento6 páginasAnalisis Pemakaian Jasa Pemasangan Gigi Tiruan Sebagian Lepasan Akrilik Pada Dokter Gigi Dan Tukang Gigi Di Desa Peuniti Banda AcehRossye MpfAún no hay calificaciones
- 023 150422122949 Conversion Gate02 PDFDocumento21 páginas023 150422122949 Conversion Gate02 PDFRossye MpfAún no hay calificaciones
- Analisis Pemakaian Jasa Pemasangan Gigi Tiruan Sebagian Lepasan Akrilik Pada Dokter Gigi Dan Tukang Gigi Di Desa Peuniti Banda AcehDocumento6 páginasAnalisis Pemakaian Jasa Pemasangan Gigi Tiruan Sebagian Lepasan Akrilik Pada Dokter Gigi Dan Tukang Gigi Di Desa Peuniti Banda AcehRossye MpfAún no hay calificaciones
- 38 116 1 PB PDFDocumento6 páginas38 116 1 PB PDFRossye MpfAún no hay calificaciones
- Diastema Closure With Direct Composite Architectural Gingival Contouring.20150306122816Documento6 páginasDiastema Closure With Direct Composite Architectural Gingival Contouring.20150306122816Rossye MpfAún no hay calificaciones
- V9n3a17 PDFDocumento6 páginasV9n3a17 PDFRossye MpfAún no hay calificaciones
- CD006968 PDFDocumento84 páginasCD006968 PDFRossye MpfAún no hay calificaciones
- 247 PDFDocumento5 páginas247 PDFRossye MpfAún no hay calificaciones
- FORM 2 Enrolment Form CTU SF 2 v.4 1Documento1 páginaFORM 2 Enrolment Form CTU SF 2 v.4 1Ivy Mie HerdaAún no hay calificaciones
- Heat and Mass Chapter 2Documento49 páginasHeat and Mass Chapter 2Mvelo PhungulaAún no hay calificaciones
- Test Bank For Macroeconomics 8th Canadian Edition Andrew AbelDocumento16 páginasTest Bank For Macroeconomics 8th Canadian Edition Andrew AbelstebinrothAún no hay calificaciones
- Fundamentals of Logistics XI - 2023Documento45 páginasFundamentals of Logistics XI - 2023saiyaAún no hay calificaciones
- Diploma Thesis-P AdamecDocumento82 páginasDiploma Thesis-P AdamecKristine Guia CastilloAún no hay calificaciones
- Study of Noise Mapping at Moolchand Road Phargang New DelhiDocumento10 páginasStudy of Noise Mapping at Moolchand Road Phargang New DelhiEditor IJTSRDAún no hay calificaciones
- Installing Go Language in UbuntuDocumento3 páginasInstalling Go Language in UbuntupanahbiruAún no hay calificaciones
- Comparison of The EC-GMP Guide Part I With The SFDA-GMP Guideline For Chinese CompaniesDocumento7 páginasComparison of The EC-GMP Guide Part I With The SFDA-GMP Guideline For Chinese Companiesrambabukomati472Aún no hay calificaciones
- P Training For ResilienceDocumento35 páginasP Training For ResilienceLbrito01100% (1)
- Pro Con ChartDocumento3 páginasPro Con Chartapi-461614875Aún no hay calificaciones
- PriceDoxy 09 September 2011Documento56 páginasPriceDoxy 09 September 2011Elena OltuAún no hay calificaciones
- Certification Programs: Service As An ExpertiseDocumento5 páginasCertification Programs: Service As An ExpertiseMaria RobAún no hay calificaciones
- On Bullshit A Problem or An OpportunityDocumento37 páginasOn Bullshit A Problem or An OpportunityEricPezoaAún no hay calificaciones
- Pre-Qin Philosophers and ThinkersDocumento22 páginasPre-Qin Philosophers and ThinkersHelder JorgeAún no hay calificaciones
- Characteristics of Victorian BritainDocumento3 páginasCharacteristics of Victorian BritainmwaqasenggAún no hay calificaciones
- Introduction To Hydraulic System in The Construction Machinery - Copy ALIDocumento2 páginasIntroduction To Hydraulic System in The Construction Machinery - Copy ALImahadAún no hay calificaciones
- Youth and Moral ValuesDocumento6 páginasYouth and Moral ValuesAlka SinghAún no hay calificaciones
- Nursing Care Plan Diabetes Mellitus Type 1Documento2 páginasNursing Care Plan Diabetes Mellitus Type 1deric85% (46)
- Koehring ManualDocumento56 páginasKoehring ManualKyle A. Nolan100% (3)
- Myplan Assessment Skills Profiler Report Summary AnalysisDocumento5 páginasMyplan Assessment Skills Profiler Report Summary Analysisapi-338283524Aún no hay calificaciones
- Stats 116 SUDocumento128 páginasStats 116 SUCAún no hay calificaciones
- ECS 3390 - Business and Technical CommuncationsDocumento293 páginasECS 3390 - Business and Technical CommuncationsEliseo Robles0% (3)
- Abbreviations For O&G IndustryDocumento38 páginasAbbreviations For O&G IndustryMike George MeyerAún no hay calificaciones
- Symbolic Interaction Theory: Nilgun Aksan, Buket Kısac, Mufit Aydın, Sumeyra DemirbukenDocumento3 páginasSymbolic Interaction Theory: Nilgun Aksan, Buket Kısac, Mufit Aydın, Sumeyra DemirbukenIgor Dutra BaptistaAún no hay calificaciones
- C779-C779M - 12 Standard Test Method For Abrasion of Horizontal Concrete SurfacesDocumento7 páginasC779-C779M - 12 Standard Test Method For Abrasion of Horizontal Concrete SurfacesFahad RedaAún no hay calificaciones
- Quick-Guide M1M 20Documento2 páginasQuick-Guide M1M 20KhaledAún no hay calificaciones
- Warranties Liabilities Patents Bids and InsuranceDocumento39 páginasWarranties Liabilities Patents Bids and InsuranceIVAN JOHN BITONAún no hay calificaciones
- Free DMAIC Checklist Template Excel DownloadDocumento5 páginasFree DMAIC Checklist Template Excel DownloadErik Leonel LucianoAún no hay calificaciones
- LPP - Problem Number 2Documento9 páginasLPP - Problem Number 2CT SunilkumarAún no hay calificaciones
- MP CRPDocumento2 páginasMP CRPankutupanaAún no hay calificaciones